All Posts by Roger Foisy
A Good Lawyer vs the Right Lawyer: How Do You Know If You Have Found the Right Lawyer?
 Navigating the complexities of a legal case can be overwhelming, no matter what your situation may be. The heart of managing those complexities is the relationship between you and your lawyer, a partnership that can influence the outcome of your case.
Navigating the complexities of a legal case can be overwhelming, no matter what your situation may be. The heart of managing those complexities is the relationship between you and your lawyer, a partnership that can influence the outcome of your case.
But in a world with hundreds of good personal injury lawyers, how do you find the right lawyer? Are all good lawyers the right lawyers? How do you avoid the wrong lawyer?
At Foisy & Associates, we understand that the ideal legal representation goes beyond legal expertise; it involves a relationship built on trust, communication, and respect. Follow these suggestions to determine if you have the best lawyer for your legal representation. Whether you are currently navigating a legal challenge or simply seeking to understand more about what makes the ideal lawyer stand out, this post is for you.
Open and Consistent Communication
One of the most important things you should be aware of when working with your lawyer is experiencing open and consistent communication. You should feel well-informed about your case’s progress and confident that your inquiries and concerns are addressed in a timely and thorough manner. The ideal lawyer who prioritizes keeping you updated via emails, meetings, or phone calls, and is readily available for discussions is often a sign of a committed and attentive legal representative.
Adherence to Deadlines
The right lawyer understands the importance of legal timelines and adheres strictly to deadlines, ensuring that all necessary documents and actions are completed well within the required timeframes. This level of organization and punctuality not only advances your case efficiently but also reflects a professional who is managing your case with the attention it deserves.
Engagement and Dedication
Feeling that your lawyer is genuinely engaged and dedicated to your case is definitely reassuring. When your lawyer shows a clear understanding of your situation, is proactive in strategy development, and demonstrates excitement in representing your interests, it shows that they are paying attention to your case and giving it the attention it deserves.
The right lawyer is one who is visibly invested in achieving the best outcome for you and who treats you not as a case but as a person. When they are dedicated to you as an individual, they clearly value your success.
Transparent Billing Practices
Transparency in billing and a clear explanation of costs associated with your case signifies that you are working with the right lawyer. A legal team that provides detailed invoices and explains billing practices upfront fosters trust and ensures that you are fully aware of how legal fees are structured and applied.
Strategic and Tailored Approach
When your lawyer has a strategic approach tailored specifically to your case, it is a positive indicator of their competence and commitment. This means they have taken the time to understand the differences in your situation and have developed a plan that maximizes the chances of a favourable outcome, demonstrating both expertise and a personalized approach to your legal needs.
At Foisy & Associates, we use a project management approach to support your case. This style ensures that you have the support, attention, and dedication from our team to ensure your case gets the settlement it deserves.
You Feel Informed and Confident
Having a lawyer who makes complex legal concepts understandable and ensures you are fully informed at every step allows you to make educated decisions about your case. The right lawyer will walk you through every step of the process and ensure you understand what is happening before they continue. This level of empowerment and confidence in your legal understanding is a key sign you are working with the right professional.
Trust and Comfort
Feeling a sense of trust and comfort with your lawyer is invaluable. This includes trusting their advice, feeling confident in their abilities, and being comfortable with their approach to your case. When you have a strong sense of confidence in your legal representation, it significantly contributes to a more positive and less stressful legal experience.
Professionalism and Mutual Respect
Experiencing a high level of professionalism and mutual respect in your interactions with your lawyer indicates a healthy and productive attorney-client relationship. This includes courteous communication, respect for your time and concerns, and professional conduct in all aspects of your case management.
At Foisy & Associates, we are dedicated to providing our clients with the highest level of legal representation and support. Our commitment to being not only the best lawyers but the right lawyers for our clients is a testament to our commitment to delivering quality results. Ready to work with our team? Contact us today for a free consultation and learn how we can help.
Roger R. Foisy, Harpreet S. Sidhu, Daniel Berman, and Rutumi Tank are experienced Ontario Personal Injury Lawyers with extensive experience in motor vehicle accidents, trips, slips, and falls, and long-term disability cases. If you have been injured in a motor vehicle accident, trip, slip, or fall, and/or your long-term disability benefits are terminated, please get in touch with us for immediate support and a free consultation.
Understanding and Advocating for Your Child: Navigating Paediatric Traumatic Brain Injuries (TBIs)
 In Ontario, head injuries stand as the number one cause of reported injuries among children aged 1-17, according to the 2019 Canadian Health Survey of Children and Youth. While many head injuries in children fortunately result in quick recoveries, the journey through a traumatic brain injury (TBI) can be fraught with uncertainty, especially considering the potential long-term impacts on a child’s development.
In Ontario, head injuries stand as the number one cause of reported injuries among children aged 1-17, according to the 2019 Canadian Health Survey of Children and Youth. While many head injuries in children fortunately result in quick recoveries, the journey through a traumatic brain injury (TBI) can be fraught with uncertainty, especially considering the potential long-term impacts on a child’s development.
In these challenging times, knowledge and compassion become invaluable allies. Understanding TBIs, recognizing their symptoms, and knowing the steps to take following an injury are crucial in advocating for your child’s well-being and securing the support and compensation they rightfully deserve.
What is a paediatric TBI?
Traumatic brain injuries, or TBIs, are a broad term used to describe a range of symptoms that differ in severity from mild to moderate to severe, occurring from both direct impacts to the head and indirect traumas.
Paediatric traumatic brain injury is not just a medical term; it represents a significant disruption in the lives of children and their families. While many children recover swiftly from TBIs, it is essential to acknowledge that for some, the road to recovery may be longer, with impacts that could last a lifetime.
Causes of TBIs in Children
The American Speech-Language-Hearing Association identifies several common causes of TBIs in children:
- Falls: Over 50% of paediatric TBIs result from falls, including slips, trips on playground equipment, or falls due to unsafe objects.
- Sports Injuries: Nearly 25% of TBIs in children occur from impacts, such as being struck by a ball or other objects.
- Motor Vehicle Accidents: Accounting for nearly 7% of TBIs in adolescents, these injuries can occur even with safety precautions like car seats and seat belts.
- Abuse: Sadly, nearly 3% of TBI cases in children are caused by assault and abuse. This includes infants who have shaken baby syndrome.
- Unknown Causes: Over 15% of TBIs in children have undetermined causes, often due to the challenges in communication with young children.
Significance of TBIs in Minors
Paediatric brain trauma, while often overshadowed by its immediate physical impact, harbours the potential for far-reaching and long-lasting risks that can significantly alter the course of a child’s life.
While a child’s brain possesses a remarkable capacity for healing, this resilience does not fully shield them from the latent dangers of TBIs. Research has shown that almost one-third (31%) of children and adolescents may grapple with persistent physical, cognitive, or emotional symptoms beyond one-month post-injury, often referred to as post-concussion syndrome.
The implications of this are profound, considering that a child’s brain continues to develop well into their mid-twenties. The disruption caused by TBIs can lead to noticeable changes in a child’s cognitive functions, emotional regulation, and overall maturity. In many cases, the full extent of these alterations may not become apparent until the child reaches an age where more complex cognitive abilities and social behaviours are expected.
Overall, the impact of a severe TBI stretches beyond the immediate aftermath, potentially influencing every aspect of a child’s life, from educational achievements to social interactions and future opportunities.
It is this deep and pervasive impact of TBIs that underscores the necessity of timely intervention and comprehensive support. Securing early and effective help is not just a matter of addressing immediate health concerns; it is a critical step in shaping a child’s long-term wellbeing and ensuring the best possible outcome for their future.
Recognizing the Signs: Symptoms of TBI in Children
Symptoms of TBIs can be subtle or pronounced, and they vary widely.
According to the Centre for Childhood Disability Research at McMaster University, symptoms of concussions (a form of traumatic brain injury) in infants and toddlers include the following:
- headache
- nausea or vomiting
- loss of balance
- disinterest in toys
- irritability
- changes in sleeping and eating habits
- fatigue
- light and noise sensitivity
Other symptoms of traumatic brain injuries in children include:
- changes in bowel and bladder function
- loss of consciousness
- impaired movement
- seizures
- visual problems
- auditory dysfunction including vertigo, tinnitus, and difficulty hearing
- Poor coordination and loss of balance
- Irritability
- Changes in sleeping habits
- And more
Immediate Steps and Legal Considerations
If you suspect your child has suffered a TBI:
- Seek medical attention immediately. A prompt and accurate diagnosis is key to recovery.
- Follow all medical advice and attend follow-up appointments. Recovery can be a gradual process requiring patience and persistence.
- Consider various treatments like physical therapy or counselling to support your child’s recovery journey.
At Foisy & Associates, we understand the complexities and challenges faced by families dealing with paediatric TBIs. If you believe your child’s TBI was caused by someone else’s negligence, we are here to support you. We will meticulously review your case and medical records and explore all avenues of compensation to ensure your child receives full and fair compensation for their injuries. This support can be pivotal in securing the financial means for your child’s future medical and therapeutic needs.
Are you or a loved one currently dealing with a potential paediatric TBI caused by negligence? Contact us for a free consultation. Foisy & Associates is a team with extensive experience in handling complex personal injury and accident benefit cases and are lawyers for the people who fight to receive maximum dollars for their clients.
Roger R. Foisy, Harpreet S. Sidhu, Daniel Berman, and Rutumi Tank are Ontario Personal Injury Lawyers with extensive experience in helping clients with brain injuries receive compensation. If you or your child has suffered a brain injury, please get in touch with us for immediate support and a free consultation.
Season’s Greetings and a Happy New Year from Foisy & Associates
 As the festive season approaches, we at Foisy & Associates wish to extend our warmest season’s greetings and best wishes for a happy new year to all. The holidays are a special time to gather with loved ones and enjoy moments of relaxation and calm. As we bid farewell to the year and welcome 2024, we encourage everyone to take this time to rest, rejuvenate, and cherish the company of family and friends.
As the festive season approaches, we at Foisy & Associates wish to extend our warmest season’s greetings and best wishes for a happy new year to all. The holidays are a special time to gather with loved ones and enjoy moments of relaxation and calm. As we bid farewell to the year and welcome 2024, we encourage everyone to take this time to rest, rejuvenate, and cherish the company of family and friends.
In the upcoming year, Foisy & Associates plans to remain dedicated to providing the highest quality service and personalized attention to each of our clients. Our focus remains steadfast on ensuring that those we represent receive the maximum disability and personal injury settlements they deserve. We are continually enhancing our skills and resources to meet and exceed your expectations in the coming year.
Holiday Hours
Please note our adjusted hours for the holiday season.
December 25-26: Closed
December 27-29: Open
January 1: Closed
January 2: Open
Our 12 Days of Christmas Giving
At Foisy & Associates, the spirit of giving is an integral part of our holiday tradition. This year, we are proud to continue our annual holiday charity practice with our “12 Days of Christmas” initiative. Each staff member at our firm contributed to a fund for purchasing gift cards, which will be distributed to twelve deserving families in our community. In a gesture of solidarity and support, Foisy & Associates matched every donation made by our team.
In addition to the gift cards, we have crafted twelve heartfelt Christmas cards to accompany the gift to these families. It is our way of spreading holiday cheer and letting them know they are in our thoughts during this festive season.
As we celebrate this season of giving and togetherness, we want to thank our clients and the community for their continued trust and support. From our family at Foisy & Associates to yours, we wish you a peaceful, joyful holiday season and a prosperous New Year.
LAT Decision Impacts Claiming Brokerage Fees for Injured Persons
 At Foisy and Associates, we are dedicated to ensuring that our clients receive the justice they deserve, especially in the realm of personal injury law. We are pleased to announce our latest victory in the case of Radebach v Intact Insurance Company, a decision that has garnered attention industry-wide for its impact and implications for future personal injury law cases.
At Foisy and Associates, we are dedicated to ensuring that our clients receive the justice they deserve, especially in the realm of personal injury law. We are pleased to announce our latest victory in the case of Radebach v Intact Insurance Company, a decision that has garnered attention industry-wide for its impact and implications for future personal injury law cases.
For those unfamiliar with the specifics of the case, Radebach v Intact Insurance Company revolved around crucial issues related to insurance claims and the rights of individuals seeking compensation, specifically regarding brokerage fees.
Insurance Companies and Brokerage Fees
For years, there have been issues with insurance providers regarding the responsibility of brokerage fees. For those unaware, brokerage fees are a cost that arises when a treatment provider (e.g. occupational therapist) is responsible for planning treatment for a client, like the organization of meetings and appointments, communicating and coordinating treatment from different providers, and more.
In catastrophic cases, insurance providers assign their claimant a case manager who takes on these responsibilities. This simplifies the case and makes it easier for the client. In these cases, the brokerage falls to the case manager to organize.
In non-catastrophic cases, insurance providers do not provide coverage for a case manager, and instead, this responsibility falls to the claimant, their family, and their medical providers to complete. When medical providers are involved in the planning and coordination of treatment like this, they charge a brokerage fee to pay for their services.
Insurance providers, however, have largely been unwilling to pay such brokerage fees. Their claim is often that because they do not pay for a case manager for non-catastrophic clients, they should not pay brokerage fees either. Instead, they have recommended that providers set aside time in their client appointments to communicate with other providers, coordinate treatments, and complete other work of this kind that is non-treatment related but is to the benefit and safety of the client. For several reasons, this is not possible or realistically achievable.
Radebach v Intact Insurance Company
In this precedent-setting case, Radebach v Intact Insurance Company, our client was denied brokerage fees, despite being a catastrophic claimant. While brokerage fees are generally accepted by insurance when charged by a case manager, in this situation the brokerage fees were charged by an occupational therapist, so the insurance provider denied the claim.
Our team decided to push this case; in most situations where we receive a case of this kind, the insurance company settles with us before the case is brought to an appeal. However, doing so also means that the insurance company continues to deny brokerage fees in the future. Our team refused to cave and pursued the appeal to finally get some answers from the License Appeal Tribunal (LAT).
We are pleased that once the appeal was heard, the adjudicator found that the request for payment of brokerage fees was deemed reasonable and necessary.
We are proud of our team’s hard work and are grateful for the support and recognition from esteemed organizations like the Ontario Rehab Alliance. In their August 2023 newsletter, the Ontario Rehab Alliance highlighted the importance of this decision, emphasizing its potential implications for future cases and the broader landscape of personal injury law in Ontario. Their recognition of our efforts and the positive outcome of this case is a testament to the dedication and expertise of our team.
This case serves as a reminder of the importance of robust legal representation in personal injury matters and the significant impact such representation can have on the lives of individuals seeking justice.
For a detailed overview of the Radebach v Intact Insurance Company decision, please visit our reported decisions page.
Are you looking for a lawyer to assist you with your LAT appeal? Contact us for a free consultation. Foisy & Associates is a team with extensive experience in handling complex personal injury and accident benefit cases and are lawyers for the people who fight to receive maximum dollars for their clients.
Roger R. Foisy, Harpreet S. Sidhu, Daniel Berman, and Rutumi Tank are Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases before the LAT and courts. They are strongly supported by Rusald Laloshi, a senior paralegal who has also represented many clients before the LAT. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
The Risks of Settling Your Entire Accident Benefits Claim
Navigating the aftermath of a motor vehicle accident can be daunting, especially when it comes to dealing with insurance claims and potential settlements. Among the various options presented to you, a ‘full and final settlement’ of your accident benefits claim is a proposal sometimes offered by your insurer after you appeal the denial of various accident benefits to the Licence Appeal Tribunal (LAT).
What does it mean to accept a full and final settlement of your accident benefits claim? How does it impact your rights as a claimant, and how can it influence your future, particularly if your injuries have long-lasting effects?
By examining what a full and final settlement is, the risks of accepting it, and how a lawyer helps you accurately assess the value of your case, you will be better prepared to navigate the complexities of your claim and protect yourself in the future.
What is a Full and Final Settlement?
A full and final settlement is an agreement you reach with your insurance provider after a motor vehicle accident. This agreement is a specified amount of money, mutually agreed upon to cover all claims for benefits – past, present, and future – that arise from the accident, as against the accident benefits insurer. These claims can encompass a variety of accident benefits from medical and rehabilitation, attendant care, housekeeping (if your injuries have been deemed Catastrophic or if optional benefits have been purchased under the policy), income replacement benefits, non-earner benefits, or caregiver benefits.
Generally, the settlement is given to you, the claimant, as a lump-sum payment and requires consent from both you and the insurer. The primary purpose of this arrangement is to provide you with closure and support while also limiting the future financial risk for your insurance provider.
Why You Should Not Agree to a Full and Final Settlement
While it may initially appear beneficial to agree to a full and final settlement of your claim with your insurance provider, it is crucial to consider the long-term implications of such a decision. When you find yourself at a LAT hearing and are offered a settlement, for instance, the future impact of your injuries might be unclear. In such a state of uncertainty, signing off on a full and final settlement implies accepting a definite sum to support your injury, eliminating any chance for further assistance down the line.
Additionally, the severity of your injuries can often be underestimated. In most cases, the full extent of damage from an accident, including the treatment you may need, such as surgery, attendant care, income replacement and other support, can take several months or even years to materialize. There is also the possibility of complications during recovery, which would require additional financial aid. It is important to envision potential future scenarios, so consider the following before agreeing to a settlement:
Will you have a permanent disability in the future?
Will you be able to perform your job effectively after your settlement?
Have you had surgery, or will you need it in the future because of your injury? If so, what are the potential risks of the surgery?
Will you need to see a therapist to deal with the mental impact and events of the accident?
What rehabilitation costs may arise in the future?
A full settlement also limits your right to pursue a determination of catastrophic impairment. This opportunity is forfeited once you’ve settled your entire accident benefits claim with your insurance provider.
Lastly, remember that while dealing with the LAT, you may find your insurer offering a full settlement for your claim even though your appeal pertains to only a portion of the claim, such as medical rehabilitation benefits or income replacement benefits. Be wary of such instances and remember, it’s crucial to think long-term when it comes to settling your claim. While a full and final settlement of your entire claim may seem appealing in the short-term, especially if you are in desperate need of treatment and/or financial support, doing so may be detrimental to your long-term health and finances if you have not considered the questions above.
How to Know What Your Case is Worth
Knowing the value of your case is critical in ensuring you receive a fair settlement. A qualified and knowledgeable lawyer, backed with experience, will provide the essential support needed to navigate your claim. A personal injury lawyer from our team will effectively assess the quality of an offer and will guide and inform you when a settlement does not align with your current and (potential) future needs.
Are you looking for a lawyer to assist you with your LAT appeal? Contact us for a free consultation. Foisy & Associates is a team with extensive experience in handling complex personal injury and accident benefit cases and are lawyers for the people who fight to receive maximum dollars for their clients.
Roger R. Foisy, Harpreet S. Sidhu, Daniel Berman, and Rutumi Tank are Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases before the LAT and courts. They are strongly supported by Rusald Laloshi, a senior paralegal who has also represented many clients before the LAT. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
Understanding Your Rights to Access Personal Information from the Police
Accessing records from the Ontario Provincial Police (OPP) or municipal police can provide crucial information for personal injury victims, particularly in motor vehicle accident cases. In Ontario, individuals have the right to request records containing their personal information, including 911 calls, from the OPP or municipal police services. However, navigating the process and understanding your rights is essential.
This post explores accessing records that contain your personal information, considerations of exemptions and personal privacy, and highlights a recent decision that illustrates the challenges and victories in obtaining this vital information.
Understanding Your Rights: Access to 911 Calls
When you have been involved in a motor vehicle accident, it is essential to understand your rights regarding access to your personal information.
In Ontario, you have the right to request records that contain your personal information from the OPP or any municipal police service. This can be a valuable resource for obtaining crucial information related to your incident. Whether you request this information yourself or through a lawyer, the process typically involves submitting a formal request form and paying a required fee.
The information you can access includes incident and investigation reports, witness statements, Crown or police briefs, records of arrest, officers’ notes, and police-related 911 calls. These records often provide valuable insights into the accident’s circumstances, aiding in understanding what transpired and supporting your case when legal action is pursued.
Exemptions and Personal Privacy
While you have the right to request access to your personal information, it is important to be aware of the exemptions outlined in the Freedom of Information and Protection of Privacy Act. These exemptions may allow the police to deny your request for specific reasons.
There are mandatory and discretionary exemptions; for example, if disclosing certain information infringes upon someone else’s privacy rights, your request may be denied.
This can create challenges when you require access to information that you did not personally provide. For instance, in a recent case we handled, we were initially denied access to 911 calls relating to our client’s incident as they were made by a third party. This highlights the potential hurdles you may encounter when seeking information that involves the actions or privacy of others.
Appealing a Denial to Access Information
Foisy & Associates recently achieved a victory in overturning the Ministry of the Solicitor General (Ministry) ‘s decision to deny access to 911 calls pertaining to our client’s motor vehicle accident. Our initial request for the 911 calls aimed to better understand our client’s injuries and state of mind immediately following the collision.
The Ministry first denied our request, citing the third-party nature of the witness’ call and the Freedom of Information and Protection of Privacy Act. However, we emphasized that our client’s interest lay solely in the information provided by the caller, not their identity or contact details. Given our client’s head injury and loss of consciousness, accessing the 911 calls would give vital insight into their well-being in the critical moments after the accident. Despite our clarification, the Ministry denied access once again.
Undeterred, we appealed the decision to the Information and Privacy Commissioner of Ontario. In a favourable outcome, it was determined that the Ministry must disclose the requested 911 calls. Since neither call contained personal information or identified the callers and considering our client’s memory loss due to their sustained injury, the calls were deemed relevant to our client’s collision. We were given access to the records.
For more information about this reported decision, please visit the reported decision’s page.
You Can Fight to Receive Information
If you have been denied information by the Ministry, it is important to know that not all hope is lost. With valid reasoning, appealing to the Information and Privacy Commissioner of Ontario may allow you access to these records.
Obtaining access to records with your personal information can be a pivotal step in gathering critical evidence to support your personal injury or long-term disability claim. As you move forward, it is crucial to have a legal team by your side that is committed to fighting for your rights and pushing for the results you deserve.
If you or someone you love has been denied benefits by your automobile insurance or long-term disability provider, we encourage you to contact us for a free consultation. Roger R. Foisy & Associates is a team with extensive experience in handling complex personal injury and long-term disability cases, and are lawyers for the people who fight to receive maximum dollars for their clients.
Roger R. Foisy, Harpreet S. Sidhu, Daniel Berman are Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases. They are strongly supported by Rusald Laloshi, a senior paralegal who has also represented many clients before the LAT. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
How to Prepare for Your LAT Hearing: 9 Steps Your Lawyer Should Take to Get You Ready
When it comes to a Licence Appeal Tribunal (LAT) hearing, preparation is key. At Foisy & Associates, we take several crucial steps to ensure our clients are well-equipped for their hearing. While the process may differ from case to case, we follow a general approach that empowers our clients to feel confident and ready for the tribunal.
A LAT hearing can be daunting, but our legal team is here to help. Learn about the steps we take to support our clients in feeling ready for their hearing.
- Understanding the process:
We start by explaining the LAT hearing process to our clients, including its purpose, structure, and potential outcomes. This helps you know what to expect and feel more at ease during the hearing. - Review the case:
Each case is reviewed with our client, going over the facts, evidence, and legal arguments. Reviewing helps clients understand the strengths and weaknesses of their case. We also discuss any potential challenges that may arise during the hearing. - Prepare documents:
We ensure that all relevant documents and evidence are organized and submitted to the Tribunal promptly. Documents submitted include medical records, expert reports, a Witness Will Say, and any other pertinent documents. - Develop a strategy:
Together with our clients, we develop a clear and concise strategy for presenting their cases. This may involve deciding which arguments to emphasize, what evidence to present, and how to best address any weaknesses in the case. - Practice testimony:
We help our clients prepare for giving testimony during the hearing. We understand this is a very stressful part of the case, so we focus our time on answering potential questions, guiding clients on how to present themselves confidently, and advising them on handling cross-examination. - Familiarize with the hearing room:
We help our clients understand what a virtual hearing will comprise of, and all the participants involved on any given day of testimony. This allows our clients to feel more comfortable and reduce anxiety on the day of the hearing. - Address logistical details:
We make sure to keep our clients informed about the schedule of the LAT hearing, which includes the specific date and time of witness testimony. Additionally, we also provide any necessary guidelines or procedures that our clients need to follow during the hearing. - Emotional support:
The LAT hearing can be an emotionally challenging experience. Our team can arrange for emotional support and reassurance, helping our clients maintain a positive attitude and confidence throughout the process. - Post-hearing follow-up:
After the LAT hearing, we will debrief with our clients, discussing how the evidence unfolded, potential next steps, anticipated waiting times for the decision rendering, and addressing any concerns or questions our clients may have.
At Foisy & Associates, we understand the challenges that come with preparing for a Licence Appeal Tribunal hearing. However, by following the steps outlined above and working with our experienced legal team, our clients can feel confident and well-prepared for their hearing. We are dedicated to providing personalized attention and support to each of our clients to ensure they receive the best possible outcome for their case.
If you or someone you love has been denied accident benefits by your automobile insurance provider, we encourage you to contact us for a free consultation. Foisy & Associates is a team with extensive experience in handling complex personal injury and long-term disability cases, and are lawyers for the people who fight to receive maximum dollars for their clients.
Roger R. Foisy, Harpreet S. Sidhu, Daniel Berman, and Rutumi Tank are Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases. They are strongly supported by Rusald Laloshi, a senior paralegal who has also represented many clients before the LAT. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
How a Project Management Approach Helps Your Case
At Foisy & Associates, we understand that personal injury and denied disability cases can have a significant impact on our clients’ lives. We recognize that our clients are often facing physical, emotional, and financial challenges, and we are committed to providing compassionate and effective representation.
Foisy & Associates operates as a project management law firm that dedicates itself to the handling of personal injury and denied disability cases while utilizing project management principles to enhance efficiency, client satisfaction, and overall case outcomes.
A project management approach in a personal injury law firm involves applying project management best practices to personal injury cases. The goal of such an approach is to ensure that clients receive effective representation and compensation for their injuries in a timely and efficient manner.
Our project management approach is not just about streamlining processes and maximizing efficiency; it’s about putting our clients first. We believe that every client deserves personalized attention and a customized strategy to achieve the best possible outcome for their case.
Key aspects of project management that we use at our law firm include the following:
- Case Management: Our firm uses project management methodologies, to streamline case processing and ensure timely completion. This involves breaking down cases into smaller tasks or milestones, assigning responsibilities to team members, and regularly reviewing progress.
- Collaboration: A strong emphasis is placed on teamwork and open communication among lawyers, paralegals, support staff, and external collaborators, such as health practitioners, medical experts, and rehab professionals. This collaboration ensures that all parties involved are working towards a common goal and staying informed about case developments.
- Client Communication: Our firm prioritizes effective and transparent communication with clients, keeping them informed of case progress, strategy decisions, and potential outcomes. This may include regular updates, meetings, or consultations to ensure that clients are fully engaged in the process.
- Resource Allocation: Our firm efficiently allocates resources, such as time, personnel, and financial commitment, to maximize the potential for successful case outcomes. This includes prioritizing cases based on their complexity, and client needs.
- Continuous Improvement: Our project management law firm is committed to evaluating and refining its processes to optimize performance continually. This might involve analyzing case outcomes, soliciting client feedback, and implementing new technologies or practices to enhance efficiency and client satisfaction.
- Risk Management: The firm proactively identifies and mitigates potential risks associated with each case, such as evidentiary challenges, legal obstacles, or financial concerns. This approach helps to improve the likelihood of success and minimize negative impacts on the client and the firm.
At Foisy & Associates, our project management approach enhances our ability to streamline case processing, maximize efficiency, and improve outcomes for our clients. Our focus on collaboration, client communication, resource allocation, continuous improvement, and risk management ensures that our clients receive personalized attention and customized strategies to achieve successful case outcomes.
By using a project management approach, we can efficiently allocate resources, proactively manage risks, and continually refine our processes to enhance efficiency and client satisfaction. This ultimately results in the timely and effective resolution of cases, saving our clients time and money.
At Foisy & Associates, we are dedicated to providing our clients with the highest level of legal representation and support. Our commitment to using project management best practices is a testament to our commitment to delivering quality results for our clients. Ready to work with our team? Contact us today for a free consultation and learn how we can help.
Roger R. Foisy, Harpreet S. Sidhu, and Daniel Berman are experienced Ontario Personal Injury Lawyers with extensive experience in motor vehicle accidents, trips, slips, and falls, and long-term disability cases. If you have been injured in a motor vehicle accident, trip, slip, or fall, and/or your long-term disability benefits are terminated, please get in touch with us for immediate support and a free consultation.
What is Catastrophic Impairment?
When an automobile accident occurs, the consequences can be life altering. For some, the injuries sustained can lead to a determination of catastrophic impairment. Understanding what catastrophic impairment is, how it’s defined in Ontario, and who makes a determination will allow you to be better prepared in the situation where you have suffered a permanent injury and believe you are catastrophically impaired.
Catastrophic impairment is a legal definition constructed by the Statutory Accident Benefits Schedule (SABS) to govern accident benefits claims. In Ontario, individuals who are considered catastrophically impaired are entitled to more substantial accident benefits than someone who experiences non-catastrophic or minor injuries.
Types of Injury Impairment
The SABS sets out three categories of injuries to determine how much money will be available to an individual after being injured in an automobile accident. Each person’s situation may differ depending on the type of benefits they have chosen, as optional benefits may entitle a person to further coverage.
Minor Injury Guideline
An individual will be classified under the Minor Injury Guideline (MIG) if they experience whiplash-related injuries, muscle strains or strains, contusions, or lacerations. An individual who falls under the MIG is entitled to $3,500 for their medical rehabilitation needs.
Non-Catastrophic Injuries
An individual who does not fall into the MIG will be classified as non-catastrophic. This typically provides up to $65,000 of medical rehabilitation and attendant care funding for up to five years from the date of the accident. For minors who have suffered injuries relating to a motor vehicle accident the duration of these benefits is funded for no more than 10 years for a minor who was 15 to 17 years old at the time of the accident; or until the minor turns 25 years old, if the minor was less than 15 years old at the time of the accident.
Catastrophic Injury
If a person has sustained more serious injuries than indicated in the MIG or non-catastrophic designations, they may meet the description of catastrophic impairment. To be found catastrophically impaired, a person must meet certain criteria as set out in the SABS.
A person who has suffered catastrophic impairment is entitled to a minimum of one million dollars over their lifetime for medical, rehabilitation, and attendant care benefits.
Catastrophic Impairment Criteria in Ontario
When determining catastrophic impairment designation, the SABS looks at impairments rather than the injury itself. The current (post-June 2016) legislation describes the following as “catastrophic impairments”:
- Paraplegia or tetraplegia that meets the following criteria:
- The insured person’s neurological recovery is such that the person’s permanent grade on the ASIA Impairment Scale can be determined.
- The insured person’s permanent grade on the ASIA Impairment Scale is or will be,
- A, B or C, or
- D, and
- the insured person’s score on the Spinal Cord Independence Measure is 0 to 5,
- the insured person requires urological surgical diversion, an implanted device, or intermittent or constant catheterization to manage a residual neurological impairment, or
- the insured person has impaired voluntary control over anorectal function that requires a bowel routine, a surgical diversion, or an implanted device.
- Severe impairment of ambulatory mobility or use of an arm, or amputation that meets one of the following criteria:
- Trans-tibial or higher amputation of a leg.
- Amputation of an arm or another impairment causing the total and permanent loss of use of an arm.
- Severe and permanent alteration of prior structure and function involving one or both legs as a result of which the insured person’s score on the Spinal Cord Independence Measure is 0 to 5.
- Loss of vision in both eyes that meets the following criteria:
- Even with the use of corrective lenses or medication,
- visual acuity in both eyes is 20/200 (6/60) or less as measured by the Snellen Chart or an equivalent chart, or
- the greatest diameter of the field of vision in both eyes is 20 degrees or less.
- The loss of vision is not attributable to non-organic causes.
- Even with the use of corrective lenses or medication,
- If the insured person was 18 years of age or older at the time of the accident, a traumatic brain injury that meets the following criteria:
- The injury shows positive findings on a computerized axial tomography scan, magnetic resonance imaging, or any other medically recognized brain diagnostic technology indicating intracranial pathology that is a result of the accident, including but not limited to, intracranial contusions or haemorrhages, diffuse axonal injury, cerebral edema, midline shift or pneumocephaly.
- When assessed in accordance with the Glasgow Outcome Scale, and the Extended Glasgow Outcome Scale the injury results in a rating of,
- Vegetative State (VS or VS*), one month or more after the accident,
- Upper Severe Disability (Upper SD or Upper SD*) or Lower Severe Disability (Lower SD or Lower SD*), six months or more after the accident, or
- Lower Moderate Disability (Lower MD or Lower MD*), one year or more after the accident.
- If the insured person was under 18 years of age at the time of the accident, a traumatic brain injury that meets one of the following criteria:
- The insured person is accepted for admission, on an in-patient basis, to a public hospital named in a Guideline with positive findings on a computerized axial tomography scan, a magnetic resonance imaging, or any other medically recognized brain diagnostic technology indicating intracranial pathology that is a result of the accident, including, but not limited to, intracranial contusions or haemorrhages, diffuse axonal injury, cerebral edema, midline shift, or pneumocephaly.
- The insured person is accepted for admission, on an in-patient basis, to a program of neurological rehabilitation in a paediatric rehabilitation facility that is a member of the Ontario Association of Children’s Rehabilitation Services.
- One month or more after the accident, the insured person’s level of neurological function does not exceed category 2 (Vegetative) on the King’s Outcome Scale for Childhood Head Injury.
- Six months or more after the accident, the insured person’s level of neurological function does not exceed category 3 (Severe disability) on the King’s Outcome Scale for Childhood Head Injury.
- Nine months or more after the accident, the insured person’s level of function remains seriously impaired such that the insured person is not age-appropriately independent and requires in-person supervision or assistance for physical, cognitive, or behavioural impairments for the majority of the insured person’s waking day.
- A physical impairment or combination of physical impairments that, in accordance with the American Medical Association’s Guides to the Evaluation of Permanent Impairment, results in 55 percent or more physical impairment of the whole person.
- A mental or behavioural impairment, excluding traumatic brain injury, determined in accordance with the rating methodology in the American Medical Association’s Guides to the Evaluation of Permanent Impairment, that, when the impairment score is combined with a physical impairment and combining requirements in the guide, results in 55 percent or more impairment of the whole person.
- An impairment that, in accordance with the American Medical Association’s Guides to the Evaluation of Permanent Impairment, results in a class 4 impairment (marked impairment) in three or more areas of function that precludes useful functioning or a class 5 impairment (extreme impairment) in one or more areas of function that precludes useful functioning, due to mental or behavioural disorder.
Determination of Catastrophic Impairment
A determination of catastrophic impairment is usually made by your insurance company at the recommendations of medical professionals. Some injuries, such as paraplegia, total loss of vision in both eyes, and complete loss of use of lower or upper extremities, are automatically deemed as catastrophic.
In most cases the injured person, or their representatives, will obtain medical opinions from experts to support the conclusion that they have reached a permanent impairment that is classified as catastrophic under the law. If the insurer disagrees with the experts, they are entitled to a second opinion and catastrophic impairment assessments from their own experts.
In cases where an insurance company and injured person do not achieve the same conclusion (i.e. one party maintains catastrophic impairment and the other disagrees), the matter will be brought before the Licence Appeal Tribunal. In this situation an adjudicator will allow both parties to present their evidence, and will make a final determination regarding the injured person’s impairment.
Obtaining a determination can be a long, drawn-out process. It is recommended that you work with a personal injury lawyer with experience in catastrophic impairment determinations and who has had experience with appearing before the Licence Appeal Tribunal. A lawyer who can effectively advocate for you and your rights can help guarantee that you are treated fairly and that you receive the appropriate determination.
If you or someone you love has been denied catastrophic impairment by your automobile insurance provider, we encourage you to contact us for a free consultation. Roger R. Foisy & Associates is a team with extensive experience in handling complex personal injury and long-term disability cases, and are lawyers for the people who fight to receive maximum dollars for their clients.
For more information on catastrophic impairment, please visit our Frequently Asked Questions page.
Roger R. Foisy, Harpreet S. Sidhu, and Daniel Berman are Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases. They are strongly supported by Rusald Laloshi, a senior paralegal who has also represented many clients before the LAT. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
The Importance of Obtaining a Lawyer Who Can Cover Expert Fees
Expert witnesses are essential to appealing a case before the License Appeal Tribunal (LAT), but they can have severe implications for your disbursements if you are not careful.
You may recall from earlier blogs that disbursements are third-party expenses you will pay following the successful resolution of your case. Disbursements are in addition to legal fees, which lawyers charge for the legal services they provide to you for a claim. Disbursements will include the cost of retaining an expert witness.
Expert witnesses specialize in their given field and will give their opinion before a court or a tribunal. A medical expert who testifies in the LAT process provides a medical opinion about an applicant’s injuries concerning a treatment plan, attendant care benefits, income replacement benefits, and even catastrophic impairment determination.
While having such expert witnesses helps bolster your case before the LAT, they can present substantial accounts for their work. Depending on the lawyer you choose, your expert fees can increase over time. Working with a lawyer who pays your expert fees quickly ensures you are not unnecessarily increasing your disbursement account—from interest on overdue accounts—which will be deducted directly from any future settlement of your accident benefits.
Table of Contents
- What do expert witnesses and third-party medical experts do for a case?
- How much do expert fees cost?
- Is the applicant the one who pays?
- Why are certain expert fees substantially higher than others?
- What happens to my expert fees if the LAT denies my appeal?
- What does Roger R. Foisy & Associates do to help?
What do expert witnesses and third-party medical experts do for a case?
When you participate in a LAT hearing, three types of witnesses participate:
- Lay witnesses, like family members and coworkers, know firsthand how an applicant’s function has been affected by the motor vehicle accident
- Treating witnesses, like family doctors, psychologists, and occupational therapists
- And Expert witnesses, who are retained by both you, the applicant, and the insurance company, the respondent
An expert witness is a person permitted to provide their expert opinion because of their unique knowledge and proficiency in a related field to the case – in LAT cases; these are often medical experts.
Expert witnesses are generally asked to answer a mix of legal and medical questions regarding your case. For example, experts may be asked to comment on a legal test or definition that an applicant has to meet to qualify for a particular benefit or to respond to whether an applicant’s requested treatment plan is considered reasonable and necessary for their injuries.
At Roger R. Foisy & Associates, we regularly use experts to comment on whether our client meets a medical-legal definition that renders them catastrophically impaired.
How much do expert fees cost?
The use of experts in a LAT appeal is an important consideration. For one, they can help you prove that a pre-existing condition did not cause your injury; or help to support the need for specific treatment and rehabilitation.
When your legal and medical team believes that your injuries from your motor vehicle accident have rendered you catastrophically impaired, insurance companies will cover up to $2,000 for a single medical expert assessment.
You will often need several expert assessments completed for a catastrophic impairment determination. Suppose you require six different assessments, which could include assessments from a neurologist, an orthopaedic surgeon, an odontologist, a psychiatrist and occupational therapists. In that case, the insurance company could pay up to $12,000 ($2,000 each) for those assessments. However, these expert assessments usually cost more – closer to $5,000-7,000 each. Applicants must realize they become responsible for the fees outside the insurance company’s payments.
If each assessor charges $7,000 and insurance covers only $2,000 of those fees, the applicant becomes responsible for the remaining $5,000 from each assessment. In our example, that would amount to $30,000 outstanding, owed by you!
Remember, though, this is only for a report regarding the determination of catastrophic impairment. Experts who testify in a LAT appeal hearing charge additional fees. Experts generally charge 1-2 hours to meet with your lawyer, 2-3 hours of individual preparation and usually testify before the LAT for half a day (3-4 hours). Depending on an expert’s hourly rate, a client can expect an expert fee to be as low as $1,200 to as high as $10,000 for testifying.
Is the applicant the one who pays?
When appealing to the LAT, we highly recommend that the applicant works with a law firm that will pay their expert fees within 30-90 days upon receipt of an expert’s invoice to avoid accruing unnecessary interest. These expert fees will become a part of the disbursements your lawyer will charge you for their services after the resolution of your case, be it a settlement or a hearing.
Why are certain expert fees substantially higher than others?
Expert fees are usually charged to a law firm upon completing the expert’s service (i.e., a medical opinion report or testimony before a tribunal). If a law firm does not have enough funds to pay the invoice immediately, the expert or law firm may often connect with a litigation loan company that will ensure their fee is paid immediately. That loan company will often act as a creditor charging interest on the invoice paid to the expert on your behalf. Upon resolving your matter, you will now be required to pay the loan company for the cost of the expert report and the interest accrued during this time. This amount becomes a disbursement which will be deducted from the overall monies you can expect to receive from any decision or settlement of your case.
In cases where litigation loan companies are not involved, experts will often charge a more significant fee if they know a law firm will take longer to pay its invoice while it waits to settle. In these situations, these increased fees also become part of your disbursements.
What happens to my expert fees if the LAT denies my appeal?
In this situation, your law firm will still use the expert information in your case outside of the LAT forum, against the person who was at fault in your vehicle accident, as the information obtained will help to win your case.
When your case is settled, the costs for these third-party expert witness fees will be claimed as a disbursement in that case and become payable from your settlement or judgment.
What does Roger R. Foisy & Associates do to help?
Roger R. Foisy & Associates does not use litigation loan companies to pay for experts. They pay each expert within a 30-90 day period from the receipt of the expert report. This ensures that the expert does not have to incorporate additional costs into the invoice. It is well understood that in the personal injury field of practice, experts who are expected to wait to be paid for their services often charge more for their legal opinions. If it takes anywhere from six months to three additional years to settle a case from the delivery of the expert opinion, how much extra will an expert be charging while they wait to be paid for their expert services?
Our law firm team members are trained to ensure that when you only obtain the services of third-party experts you require to prove your claim, you will not pay for more expert assistance than you need. Our lawyers use strategy and consider the many factors of your case to decide when and whom we obtain as third-party experts. We do not treat you as part of a transaction but prioritize working on your case as effectively as possible.
We pledge that the job is done right, and our project management processes save you money in the long term. Our methods to keep you from paying extensive and unnecessary expert fees can help you save tens of thousands of dollars in disbursements.
Are you looking for a lawyer to assist you with your LAT appeal? Contact us for a free consultation. Roger R. Foisy & Associates is a team with extensive experience in handling complex personal injury and accident benefit cases and are lawyers for the people who fight to receive maximum dollars for their clients.
Roger R. Foisy, Harpreet S. Sidhu, and Daniel Berman are Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases before the LAT and courts. They are strongly supported by Rusald Laloshi, a senior paralegal who has also represented many clients before the LAT. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
Having the Right Legal Representation for the LAT
If you need to go through the Licence Appeal Tribunal (LAT), it is essential to have a representative who can effectively advocate for you and protect your rights and interests. Without legal representation, you may be at a disadvantage and may struggle to present your case effectively. Although it is possible to represent yourself before the LAT, it is usually in your best interests to seek legal counsel to ensure that you are treated fairly and your rights are protected.
What is the Licence Appeal Tribunal?
The LAT is a quasi-judicial agency that reviews applications and resolves disputes related to compensation claims and licensing activities. It is composed of two divisions: the General Service division and the Automotive Accident Benefits Service (AABS). These divisions provide adjudicators who review appeals and try to resolve disputes between claimants and insurance providers.
For more information about the LAT, visit our LAT resources page.
Why do I need legal representation for the LAT?
Technically, you are not required to have a legal representative when you appear before the LAT.
At Roger R. Foisy & Associates, we strongly recommend that you retain the services of a legal representative, whether that be a paralegal or lawyer. Both paralegals and lawyers are governed by the same laws and principles, but there are some differences between the two types of legal representation.
Paralegals may seem to be a more affordable option than a lawyer, however in this area of law paralegals and lawyers charge the same or very similar contingency fee rates. It is important to note that paralegals are restricted in the types of benefits they can dispute before the LAT. Lawyers are able to represent clients in a wider range of case situations, specifically disputes involving the determination of catastrophic impairment.
If you have suffered serious injuries, it is especially important to hire an experienced lawyer who can effectively argue your case before the LAT. At Roger R. Foisy & Associates, we have worked extensively with the LAT and are confident in our lawyers’ ability to achieve the maximum compensation for our clients.
Why should I use a lawyer when I appear before the LAT?
The best choice for your advocate is one who understands the LAT and can represent you no matter your situation.
For effective advocacy before the LAT, you should strongly consider using a lawyer with experience and a thorough understanding of the regulatory framework and behaviours during an appeal. Your lawyer should have experience appearing before the LAT, including the completion of oral hearings. An experienced lawyer will have examined and cross-examined lay witnesses, treating witnesses and expert witnesses.
More importantly, an experienced lawyer will be able to guide you through the process where the opportunity of a fair and reasonable settlement can be achieved. However, if an insurance company is unwilling to settle, an experienced lawyer will be able to properly represent you at the LAT hearing.
Additional Costs
Depending on the type of appeal you are advancing, your case may also require additional costs.
If you are appearing before the LAT for complex issues like income replacement benefits, attendant care benefits, or the determination of catastrophic impairment, you will need expert witnesses to provide the information you need to win your case.
Experts require payment for their reports as well as their testimony if they are to appear as an expert on your behalf at an oral hearing at the LAT. Some law firms including ours will advance the costs associated with hiring expert witnesses for your case, which can vary between $25,000-$35,000.
In these situations, your law firm requires the financial means to handle the expenses of third-party medical reports and expert testimony.
It is important to understand that the law firm you hire is prepared to fund these expenses in the event you are required to appeal your insurance company’s denial of your accident benefits.
If you or someone you love has been denied benefits by your automobile insurance provider, we encourage you to contact us for a free consultation. Roger R. Foisy & Associates is a team with extensive experience in handling complex personal injury and long-term disability cases, and are lawyers for the people who fight to receive maximum dollars for their clients.
Roger R. Foisy, Harpreet S. Sidhu, and Daniel Berman are Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases. They are strongly supported by Rusald Laloshi, a senior paralegal who has also represented many clients before the LAT. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
Merry Christmas & Happy New Year!
 The team at Roger R. Foisy & Associates would like to wish you and your loved ones a Merry Christmas and a Happy New Year! We hope your holiday season is filled with good company, good food, and plenty of relaxation. May you take this time to reflect on the year and look forward to what 2023 brings.
The team at Roger R. Foisy & Associates would like to wish you and your loved ones a Merry Christmas and a Happy New Year! We hope your holiday season is filled with good company, good food, and plenty of relaxation. May you take this time to reflect on the year and look forward to what 2023 brings.
As we look ahead, our team remains committed to providing every client with personalized attention and quality service, as well as working our hardest to ensure clients receive maximized disability and personal injury settlements.
Holiday Hours
December 23: Open
December 24-27: Closed
December 28-30: Open
December 31-January 2: Closed
January 3: Open
A Holiday Season for Giving
Our firm has an annual practice of giving during the holiday season; this year, our staff members will be donating money to go towards purchasing gas and grocery gift cards to be given to the less fortunate. Our firm will be matching all donations made by our team.
Team members will also be designing and making holiday cards, which will be sent with these gift cards to individuals in need.
Season’s Greetings from Roger R. Foisy & Associates to you and your loved ones!
Roger R. Foisy to Speak at CSME Webinar
Roger R. Foisy has been invited to speak at an upcoming webinar for the Canadian Society of Medical Evaluators (CSME) this December 1st, 2022. The webinar will discuss Tips and Strategies when Testifying for Occupational Therapy and Functional Abilities Evaluations.
This webinar will identify to occupational therapists and other medical evaluators how to provide information clearly and objectively when testifying at trial to ensure that you appear credible and make sure the trier of fact will consider your testimony.
Information will focus on functional and in-home evaluations and be relevant to all disciplines when testifying.
Roger will be joined as a presenter at this seminar by Louis Zavodni, clinical director and owner of Total Healthcare Solutions, and Stacey Baboulas, occupational therapist and owner of Stacey Baboulas & Associates. This webinar will be moderated by Dr. Rhonda Nemeth, Ph.D., C. Psych., CMLE (O), C-CAT (MB) of the CSME.
The CSME is the leading national organization of professionals involved in independent medicolegal and clinicolegal evaluations using evidence-based medicine and best clinical practices.
For more information or to register for this webinar, please visit the CSME website. Registration is available for both members and non-members of the CSME.
Roger R. Foisy, Harpreet S. Sidhu, and Daniel Berman are experienced Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
Always bring a combination square with you! The importance of proper tools while using municipal sidewalks
Trips, slips, and falls are common sources of litigation for municipalities. Ensuring that sidewalks are in a state of good repair and are not impacted by poor weather conditions or damage is part of the regular maintenance that must be completed.
If you have been injured from a slip, trip, and fall due to ice or snow in Ontario, you must act quickly to provide written notice. You have only ten days to provide written notice to municipalities if the fall occurred on a municipal sidewalk or roadway, and only 60 days to provide written notice to the property owner or responsible maintenance contractor for all other properties. For more information about this, please read our blog discussing this policy.
To help protect yourself, it is important to follow certain practices: wear boots in the winter and running shoes if you are out for a run. But what about carrying professional measuring tools?
We wish to raise awareness of a recent court decision, in the case of Cromarty vs Waterloo (City). In this case, the plaintiff fell on the municipal sidewalk that she regularly travels. Two weeks later, the plaintiff and her son-in-law returned to the location to re-examine the area.
They took photographs of the location and measured the height difference between the two sidewalk slabs where she fell. The measurements were taken with a makeshift tool, composed of a piece of cardboard and a ruler. With their tool they found that the difference between the blocks was 20-25 mm.
Two separate investigators were assigned to determine the height difference in this case, who utilized a combination square to determine the difference in sidewalk block heights. These investigators determined that the difference was closer to 17.5-18.5 mm – a difference of 1.5-6.5 mm from the plaintiff’s tool.
It was determined by the court that using a makeshift measurement is an inaccurate way to determine a state of disrepair.
Justice Broad noted that “a ruler used alone is an inferior device to a combination square for the purpose of measuring height differentials between two horizontal planes.” It was instead suggested that taking measurements with a combination square is the appropriate and reliable method to measure surface discontinuity.
With these results, we thought it would be important to recommend and suggest that you purchase a combination square to carry for personal use in case you fall and need to measure the surface discontinuity where you took a tumble, without delay.
Remember, only with the use of a combination square can we protect ourselves from inaccurate measurements.
Roger R. Foisy, Harpreet S. Sidhu, and Daniel Berman are experienced Ontario Personal Injury Lawyers with extensive experience in motor vehicle accidents, trips, slips, and falls, and long-term disability cases. If you have been injured in a motor vehicle accident, trip, slip, or fall, and/or your long-term disability benefits are terminated, please get in touch with us for immediate support and a free consultation.
Roger R. Foisy Invited as Speaker at 2022 OTLA Fall Conference
Roger R. Foisy has been invited to participate as a speaker at the Ontario Trial Lawyers Association (OTLA) 2022 Fall Conference. The conference theme this year is The Pressures of Practice.
Roger will be participating in a presentation discussing the topic of “An In-depth Analysis of Why the Plaintiff Bar is Shouldering the Out of Hand Cost for Disbursements”. Roger is regularly invited to speak at OTLA and other organizations on topics relating to Practice Management, Personal Injury, and Long-Term Disability.
The event is scheduled for October 28, 2022, is exclusive to OTLA members. To register, please visit the OTLA website.
The OTLA is a non-profit professional association for plaintiff lawyers and staff with over 1400 members across Ontario, other provinces, and the US. By offering training, enhancing access to justice, promoting and advocating for full and just protection, and offering practical solutions to improve the legal system, the OTLA works to advocate for the rights of those who have suffered injury and loss due to the wrongdoing of others.
Roger R. Foisy, Harpreet S. Sidhu, and Daniel Berman are experienced Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
World Mental Health Day: Recognizing the Psychological Fallout of Motor Vehicle Accidents
World Mental Health Day is an international day for mental health education, awareness, and advocacy, celebrated on October 10th each year. Originally created in 1992, this day helps raise awareness and bring attention to mental illness and its effects on people’s lives worldwide.
While we often recognize that psychological disorders can be pre-existing or caused by stress, many don’t consider the impact that motor vehicle accidents can have on a person’s mental health. Motor vehicle accidents are typically thought of as causing physical injury and damage to the person. However, psychological conditions can arise after an accident — even if it is not serious.
In a 2021 study completed it was found that survivors of motor vehicle accidents reported substantial rates of mental health problems, with 32.3% suffering from post-traumatic stress disorder (PTSD), 17.4% suffering from depression, and 5.8% suffering from anxiety.
It is important to recognize that motor vehicle accidents can cause physical, cognitive, and psychological damages, for which victims can be entitled to coverage.
The Psychological Fallout of Motor Vehicle Accidents
As a personal injury law firm, we see the devastating impact that motor vehicle accidents can have on individuals and their families. We understand how important it is for victims to be able to recover from their injuries, whether physical or mental.
Unfortunately, there is still a stigma around those who suffer from mental health issues like PTSD. This can prevent people from coming forward after an accident and seeking help.
It is time to change this. We need to raise awareness about PTSD, depression, and other ailments and how they can affect people who are involved in motor vehicle accidents. We want our clients to know that they are not alone and that we are here for them every step of the way.
Can you claim psychological damages after a car accident?
Sometimes, a motor vehicle injury can lead to a severe psychological illness. If your condition is causing you to be unable to work or carry out housework, you can claim monetary losses for your psychological damages. Non-monetary losses can also be claimed, such as difficulty interacting with others, a distraction from enjoying life, and other symptoms.
Roger R. Foisy and Associates understand the challenges facing individuals who experience these types of disabilities. We take a special approach to handling psychological or psychiatric disability cases.
Settling Mental Health Claims
Every legal case has its own circumstances and with that, individual considerations. Determining whether one should settle their claim requires the understanding of an entire case to give accurate insight.
Settling motor vehicle accident benefits for an amount of money which usually is within the $65,000 maximum when it comes to medical, rehab, and attendant care benefits may prove to be problematic if over time your injuries worsen and can still be traced back to their original cause.
It is important to remember that as a person’s physical or cognitive injuries fail to improve and become chronic, their mental and behavioural state can also become debilitating.
Suppose that condition on its own results in an accident victim becoming markedly impaired in three of four areas (activities of daily living, social functioning, concentration, persistence and pace or adaptation), or extremely impaired in one of the same four areas. In that case, that person could later be deemed catastrophically impaired.
The law also recognizes a combination of physical, cognitive, and mental behavioural whole person impairment of at least 55% (with 53% rounding up to 55%) resulting in a person being deemed catastrophically impaired.
For more information on catastrophic injury coverage, read our blog regarding optional benefits and how they can protect you in case of a motor vehicle accident.
If you or someone you know has been involved in a motor vehicle accident, contact a personal injury lawyer immediately. A lawyer can help you assess the situation and make decisions about filing a claim against the person responsible for the accident.
Roger R. Foisy, Harpreet S. Sidhu, and Daniel Berman are experienced Ontario Personal Injury Lawyers with extensive experience in motor vehicle accident cases. If you have been injured in a motor vehicle accident, please get in touch with us for immediate support and a free consultation.
Using Structured Settlement to Help Those Who Suffer From Traumatic Brain Injuries
 People who suffer from traumatic brain injury, or TBI, face a different world than the everyday person. A person who has a TBI is more likely to suffer from mental health issues and is also more likely to experience unemployment, homelessness, and in some cases incarceration.
People who suffer from traumatic brain injury, or TBI, face a different world than the everyday person. A person who has a TBI is more likely to suffer from mental health issues and is also more likely to experience unemployment, homelessness, and in some cases incarceration.
TBI is a traumatic experience – those who suffer are forced to change their lives dramatically to find a new quality of life and adjust to their new reality, which can be a struggle. Where they once were able to complete simple tasks on their own, they may have to rely on others, and often lose a sense of independence in their life.
In Canada, when negotiating a settlement for a person who has suffered a brain injury, a structured settlement is often used to provide more benefits for the plaintiff. Structured settlements can offer a better quality of life and make it easier to manage financial stability for the recipient.
What is a traumatic brain injury?
A traumatic brain injury, or TBI, is a form of brain injury that occurs when a sudden trauma causes damage to the brain.
Traumas that may cause a TBI include hitting one’s head on a hard surface after a trip or fall or a motor vehicle collision where the head is struck on the interior of the car, or by force of a deploying air bag. However, it is imperative to note that a direct impact to the head is not required for a TBI to occur. Rather, a simple whiplash motion (e.g. from a rear-end collision), can cause a TBI as well.
Traumatic brain injuries cause many challenges, including issues with muscle coordination, memory, emotional control, dizziness, fatigue, headaches, ringing in the ears, reduced focus and concentration, and paralysis. For more information, please read our blog discussing the symptoms and effects of a TBI.
What is a structured settlement?
A structured settlement is an agreement for the payment of damages in a personal injury lawsuit, where the payments are made over time. These payments are guaranteed, tax-free deposits that can last either across a plaintiff’s lifetime or until a determined period.
These payments can be preferable to traditional payouts because it allows the plaintiff to receive their compensation in a way that is easier to manage their finances over time. Some people also prefer structured settlements to lump sum payouts because they know exactly how much money they will receive each month and can better prepare for when the payments stop (if not paid to lifetime). Importantly, the amount structured will also earn interest, tax-free, which will have the effect of growing the settlement amount for the duration of the structure.
How does a structured settlement help those with a TBI?
In the event of a TBI, an individual may need to rely on a structured settlement to pay for their care. This will allow those who have suffered from a TBI to build independent structures in their life, as well as increase their financial stability. This can be beneficial for several reasons:
It allows the injured person to receive compensation while they are still recovering. This may allow them to purchase additional services or equipment that their insurance might not cover or pay for. It also allows them time to adjust their lifestyle around their injuries and begin saving for future needs.
It gives the injured person more control over how their money is spent. This can help keep them from making decisions based on emotions or impulse that could lead them into financial trouble later down the line.
It avoids any tax liability for the plaintiff. If the plaintiff receives money from an injury settlement, it is not considered taxable income and they will not owe taxes on it.
Structured settlements can work out well for those who have suffered from a TBI. By allowing them to focus on their quality of life, rather than their finances, structured settlements can provide a better foundation for a person who has suffered a TBI.
Roger R. Foisy and Harpreet S. Sidhu are experienced Personal Injury Lawyers in Ontario who have helped clients with brain injuries receive compensation. If you or a loved one has suffered a brain injury, please contact us for immediate support and a free consultation.
Thank You for Attending the 2022 BIAPH Health Advocate Education Conference
Roger R. Foisy and Associates would like to thank all who came to The Brain Injury Association of Peel and Halton’s (BIAPH) 3rd Health Advocates Education Conference.
Hosted on June 29, 2022, at the Mississauga Convention Centre, the theme this year was Practical Tips and Strategies from Industry Professionals and featured several 10–15-minute presentations from health advocates, legal professionals, and insurers focused on providing insight and knowledge that all professionals can use to help their clients.
In addition to presentations, the conference also offered the opportunity to promote and connect with other healthcare and rehabilitation professionals and advocates.
We would like to thank our team specifically who helped to organize the event, the amazing sponsors who helped to support the conference, and all attendees who made the Health Advocate Education Conference such a success.
BIAPH is a non-profit organization that exists for the needs of families and survivors of brain injury in the Peel and Halton Regions. BIAPH facilitates measures to promote the prevention of brain injury, improve quality/care of life, provide community education, and conduct resource searches on behalf of members.
We look forward to the next conference in 2024 and hope to see you there.
If you are looking for assistance with a serious personal injury matter or navigating your long-term disability insurance claim after it has been denied or terminated, Roger R. Foisy & Associates can assist you. Contact us for a free consultation to find out how we can help.
Verify Your Home Insurance Coverage & Protect Your Assets in Case of an Accident
On June 5, 2022, one of the staff of Roger R. Foisy faced tragedy as she lost her entire home to an apartment building fire. She and her two children were left with only the clothes on their back as they faced damage and unfortunately were not able to return to their home.
As we see the personal impact of accidents and the dangers of losing your belongings, we wanted to encourage everyone to take the time to review their home insurance policy. Ensure that you have enough insurance to cover your belongings and the correct insurance for your possessions. Depending on the types of accidents that may occur, it is important to make sure you are protected from certain damage like floods or sewage, which have special coverage limits.
With this reminder, it is also important to make an inventory note of the valuables you have in your home. Making sure you have a record of the exact property you own ensures that you can obtain the correct assets with as little difficulty as possible.
Verify Your Home Insurance Coverage
Home insurance is there to protect you and your family in the event of an accident, fire, or robbery. It is important to make sure that your home insurance coverage is up to date, otherwise, you could end up being underinsured and vulnerable to financial losses.
Checking your home insurance coverage on a regular basis can help ensure that you are adequately protected in the event of an unexpected incident. Here are a few tips for checking your home insurance coverage:
- Make sure that your policy covers all your personal belongings. This includes items such as jewelry, art, and electronics.
- Consider increasing your protection if you have recently made improvements to your home, such as adding a new extension or renovating an older property.
- Check what protection is included in case of accidental damage, such as fire or flooding. You may need to purchase additional coverage if you live in an area at risk of these hazards.
- Make sure that you are aware of any exclusions in your policy. For example, many policies will not cover damage caused by earthquakes or floods.
By taking the time to check your home insurance coverage, you can be sure that you and your family are adequately protected in the event of an unexpected incident.
Inventory of Valuables
If you own valuable items, it’s important to document them for insurance purposes. If your home is damaged by fire or flooding, or if you are the victim of a robbery, having a detailed list of your possessions will make it easier to file a claim and receive compensation from your insurance company. To create an accurate inventory, follow these suggestions:
- Take photos or videos of each item and make note of any distinguishing features.
- Consider taking a video of all your belongings, and not just your valuables. This will help you identify the exact items you possess in case of loss, and better guarantee that when insurance replaces those items, they are the same or of equal quality.
- Update your lists regularly as you acquire new items.
- Make sure to open drawers and closets as you record your belongings. We often forget to make notes of items that have been put away.
- Save copies of receipts, appraisals, videos, and photos in an online cloud as a backup in case you cannot access them. This will guarantee you are able to provide your insurance company information despite your losses.
We recommend that you consider reviewing your home insurance coverage and taking inventory of your belongings on an annual basis. Choosing an easy-to-remember date like Fire Prevention Week (the week of October 9) and making a note in your calendar can help you ensure you are adequately compensated if the worst should happen.
Roger R. Foisy & Associates would like to thank members of the community who made donations and contributed their time to help our staff member in their time of need.
If you have sustained a personal injury or disability, please contact Roger R. Foisy & Associates for a free consultation or call us at (905) 286-0050.
Why You Need Optional Benefits in Your Ontario Automobile Insurance Policy
 On June 1, 2016, Ontario changed the benefits for automobile insurance, making adjustments that limit your access to long-term medical and rehabilitation benefits. This change was made quietly, and the people of Ontario were uninformed about the amendments made to their insurance policies.
On June 1, 2016, Ontario changed the benefits for automobile insurance, making adjustments that limit your access to long-term medical and rehabilitation benefits. This change was made quietly, and the people of Ontario were uninformed about the amendments made to their insurance policies.
These changes were silent but created serious consequences, leaving thousands of Ontarians affected since June 2016.
Meet Adam
Adam* purchased automobile insurance in August of 2016 thinking he had coverage that would protect him from any injuries he may obtain in the event of a motor vehicle accident.
Like every Ontarian, Adam shopped around. He knew it was mandatory to have coverage but wanted to save money, so he purchased the standard policy at the best price he could find and assumed he had the best protection available. He did not know to ask any further questions, nor did his broker make him aware of additional options available.
When Adam got into an accident in March 2017, he suffered serious injuries which were deemed non-catastrophic by his insurer. Under the new benefits limits, that meant Adam would be eligible for a maximum of $65,000 of medical rehabilitation and attendant care coverage for a fixed period of five years – whichever came first. Between his auto insurance coverage, work benefits plan, and OHIP, he and his family assumed he would be able to fully pay for the rehabilitation support he needed for as long as it took for him to recover.
Shouldn’t OHIP and work benefits have covered that?
As Adam worked on his recovery the money quickly dwindled. Adam, like many Ontarians, thought that OHIP would cover him for any costs required for treatment, with his auto policy and work benefits paying for the difference. However, he soon realized that funding through his work benefits was limited, as was the protection provided by OHIP. In fact, the majority of the treatment he needed for recovery was only available through private clinics and had to be paid for by his auto policy.
 When he turned to OHIP, he was permitted 4 hours per day of personal support care. His work benefits provided no coverage for personal support care, and so he was left without support for 20 hours per day.
When he turned to OHIP, he was permitted 4 hours per day of personal support care. His work benefits provided no coverage for personal support care, and so he was left without support for 20 hours per day.
His wife was able to take a few days off work to assist him, however, he would require aid for a 3-month period. His wife was unable to take that much time from work, and so they had to find another option.
When Adam turned to his auto insurer, he learned that he was entitled to a maximum of $3,000 a month for the assistance of a Personal Support Worker (PSW) at the hourly rates set by the provincial regulations for persons injured in an auto accident.
With the actual current rate of $40 per hour, this only gave him 75 hours of attendant care per month versus the over 700 hours per month that he actually required – particularly in the first three months when he was immobile and unable to perform basic tasks for himself.
Assuming that the insurance company paid him the $3,000 a month for treatment, Adam would have used $9,000 out of the $65,000 available from his policy just on the minimal amount of attendant care support he received. Before Adam had even begun treatment, he had used up 14% of his total benefits available to him over the five-year coverage period.
Adam now needed to pay for regular physiotherapy, massage therapy, and rehabilitation therapy to begin his recovery. His employee benefits covered the first $300 of each type of therapy, but that was not going to be nearly enough.
Because of the injuries that made him non-weight bearing, Adam’s physiotherapy was in-home for the first month, followed by in-clinic treatment for months afterward. Considering that the average in-home physiotherapy session cost is $100 (plus travel time for in-home care) and that he needed 2-3 sessions per week for the near future – never mind the other types of therapy he needed, plus medication – Adam began to realize how little coverage he had.
The Five-Year Limit Surprise
Worst of all as Adam began his recovery, he quickly understood that it would not take weeks or even months, but rather years to heal. In fact, some injuries would require a lifetime of therapy to allow him to function adequately at home and, when he eventually returned, at work.
He learned that the term “non-catastrophic” was an insurance term that did not reflect the reality of his situation which felt catastrophic and life-altering to him.
Because Adam did not buy the optional benefits that would have provided him with $1 million of LIFETIME coverage for non-catastrophic injuries, he discovered, to his surprise, that his insurance company’s financial assistance would only last him for five years, or when the limited non-catastrophic medical rehabilitation benefits of $65,000 were depleted. His injuries, however, would last him forever.
Adam was forced to either give up on many parts of his recovery, trying to spread out the remaining funds over the next four years or pay thousands of dollars out of pocket. He simply could not afford to go on with therapy the way that he wanted. His life was changed forever, and insurance was not able to help.
Very often, in other cases, the five years runs out before money does, creating a very heavy financial burden on the injured person and their family over the injured person’s lifetime.
 What Might Have Been
What Might Have Been
If Adam had been made aware, by his insurer or broker, of the available optional benefits, things would have been very different. For around $100 a year, he could have protected himself for life with access to up to $1 million for non-catastrophic Medical Rehabilitation Benefits and $3 million if he was deemed catastrophic.
Adam made an easy mistake. He was uninformed and thought that he was making the best decision.
Why did Adam not know? Most people shop based on price and our clients tell us that their brokers and insurance companies did not take the time to explain optional benefits to them. Without the information necessary to make an informed decision, most people choose a standard policy without knowing the risks.
Are you protecting yourself?
Since June 1, 2016 hundreds of thousands suffered personal injuries while in an automobile accident in Ontario. If you or your family ever take trips on the highway, visit family, or commute to work, it is imperative to include optional benefits in your automobile insurance policy.
June 1, 2016, is known by many personal injury lawyers as Doomsday because of the impact it had on their clients and how many lives have been altered due to Ontario’s changes to automobile insurance. These changes have put the responsibility on YOU to be aware of optional benefits and how important they are to protect yourself and your family.
What changes have been made?
Before the adjustment, regular benefits provided the following:
- medical rehabilitation benefits of $50,000 for ten years
- attendant care benefits for $36,000 for ten years
- catastrophic injury benefits for medical and rehabilitation needs of $1 million for life
- attendant care of $1 million for life
With the June 2016 update, regular automobile benefits have been changed to offer the following:
- medical rehabilitation and attendant care benefits have merged and reduced to $65,000 for five years
- the catastrophic medical rehabilitation and attendant care benefits have merged to provide $1 million in total for Life Expectancy
These changes have been made to simplify things for auto insurance companies but provide you with less support and coverage. What are you supposed to do?
The best way to protect yourself and your dependants is by signing up for optional benefits.
The chart below illustrates the optional Medical Rehabilitation Benefits available to you and the estimated annual costs.
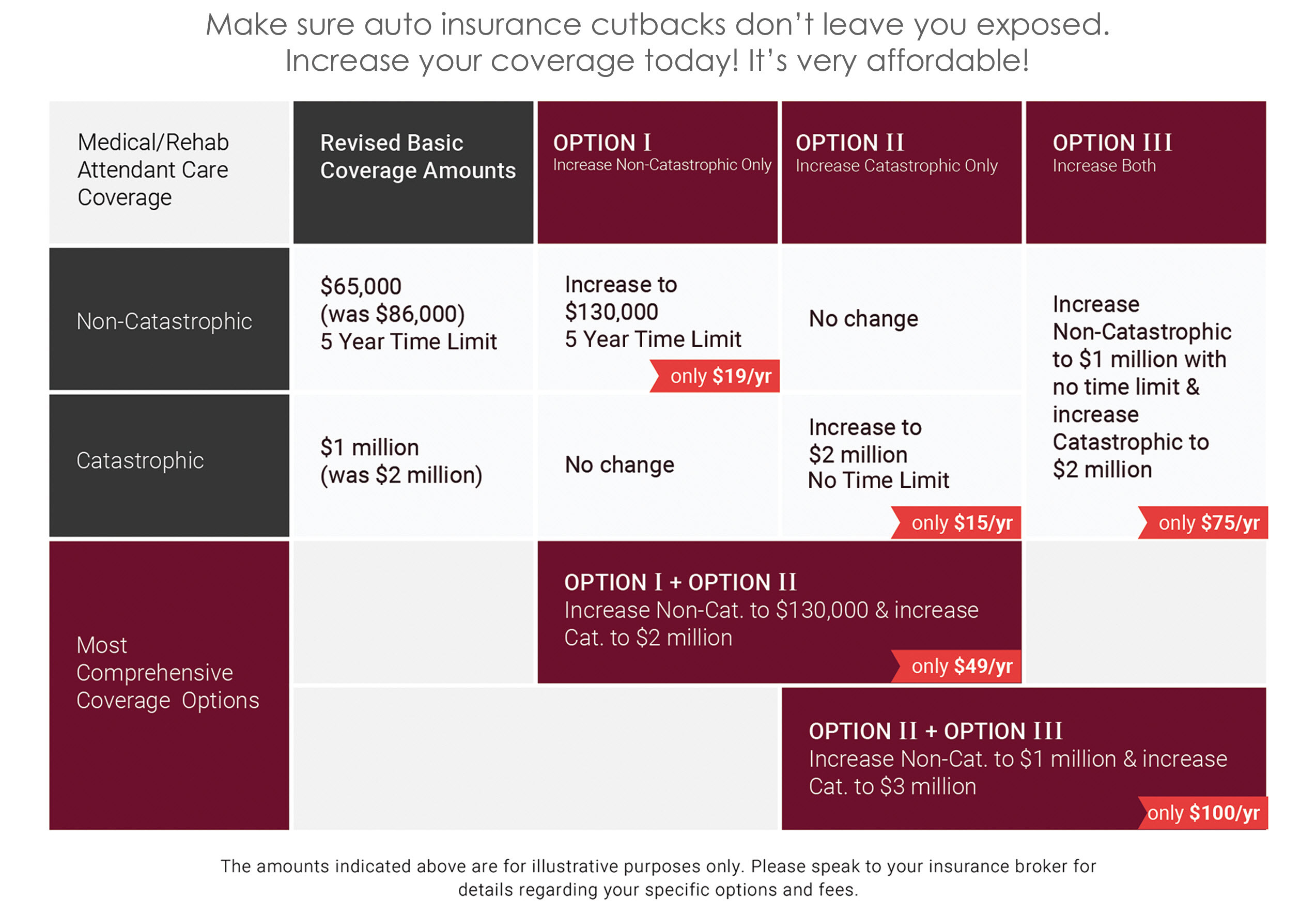
Download chart in PDF to discuss with your insurer or broker.
What do optional benefits provide?
For an additional $100 a year**, you can adjust the coverage you receive in every situation.
Increase in Benefits
Adding optional benefits for non-catastrophic injuries provides $1 million in coverage for all medical, rehabilitation, and attendant care benefits needs – up from $65,000 for standard benefits.
You will also increase your support to $3 million for catastrophic injuries – up from $1 million for standard benefits. For catastrophic injuries, particularly if you are still of working age and have financial responsibilities, $1 million is not nearly enough for your support and recovery.
Protection for Dependants
It is important to note that the automobile benefits that you have carry across for not only yourself and your vehicle, but your dependants as well. Purchasing the right insurance means keeping yourself and your family protected no matter what happens.
Lifetime Coverage
As we discussed earlier in the case of Adam’s “non-catastrophic” injuries, $65,000 was only going to be available for five years, assuming the money lasted that long. In many other cases, there are funds left over when the five years expire, despite needing to continue treatment. Optional benefits last for life.
While $1 million for catastrophic injuries sounds like a lot of money, the concern lies in the five year time limit to use the money available rather than just how much your insurance offers you financially. If it is not used in the five years of support offered, it is gone.
By definition, catastrophic injuries are just that – catastrophic. In our experience, the physical, emotional, and psychological problems do not go away in five years. Furthermore, you could try a different career ten years after your accident, bringing out an old injury, and need physiotherapy to help adjust.
These injuries will impact you for the rest of your life – your insurance should protect you for life, too.
How do I get optional benefits?


Ask Your Insurer/Broker Questions
There is nothing wrong with shopping for the best price on your automobile insurance. However, once you have the best price, ask the insurer or broker to add the maximum optional Medical Rehabilitation Benefits available. Ask for non-catastrophic coverage of $1 million and catastrophic coverage of $3 million. You will be shocked to find out that only a few extra dollars per month will provide so much more coverage for you and your family.
For those who are intimidated, we encourage you to download our helpful chart to send to your insurer or broker. We have also put together two questions to ask your current insurer or broker:
- Does my policy or quote include maximum optional benefits for non-catastrophic Medical Rehabilitation Attendant Care and catastrophic benefits for life?
- If not, how much will it cost to add the optional $1 million non-catastrophic Medical Rehabilitation Attendant Care (M/R/AC) benefit for life AND the $3 million (M/R/AC) catastrophic benefit for life?
Then ask yourself: for the additional few dollars a month, can I afford NOT to protect myself and my family for life in the event of an accident?
Find the Right Insurer/Broker
A good insurer or broker will be able to provide insight on how to integrate optional benefits into your plan. Be sure to give them time to answer your questions – some may not have the information about optional benefits that you need immediately, since this change was so swept up under the rug. If you do not get the answers you need, however, consider shopping around for another insurer or broker who will advocate for you.
Once you have added the optional benefits to your plan, ask your broker to show them to you in your policy. This way you can guarantee that your benefits are there, and they are not missed.
Optional Benefits Create Peace of Mind
While there are several types of benefits and features that you can add to your policy, we encourage you to choose the highest optional benefits for Medical Rehabilitation Attendant Care offered. The peace of mind provided by guaranteeing lifelong coverage is the best support you can ask for.
Share this blog with others who might not be aware to help them better understand how they can protect themselves.
Consider also providing these benefits to others who may not know the available options. What better gift to provide your parents for Christmas, or your children who are just starting a family? Peace of mind is a better present than another gift card, or worse: another cologne.
If you have sustained a personal injury or disability, contact Foisy and Associates for a free consultation to find out how we can help.
*Real name has been changed for confidentiality
**Rates may vary depending on your provider.
Roger R. Foisy Invited as Panelist on OTLA Long-Term Disability Roundtable
Roger R. Foisy has been invited to participate as a panelist on the Ontario Trial Lawyers Association (OTLA) roundtable on Examination for Discovery of an LTD Defendant.
Other prominent lawyers who will be part of the panel include Nainesh Kotak, Steve Rastin, and Najma Rashid.
Roger is regularly invited to speak at OTLA and other organizations on topics relating to Long-Term Disability, Personal Injury, and Practice Management.
The 60-minute in depth roundtable will focus on the defendant discovery in LTD cases. Topics discussed will include:
- Timing of discovery
- Who to examine?
- Preparation
- Areas of questioning
- Refusals and undertakings
- The use of Simplified Rules
The event scheduled for March 2, 2022, is exclusive to OTLA LTD section members and is free to attend.
Does Your Union Insurance Policy Cover Long-Term Care?
If you are an active or retired union member, your insurance policy might cover long-term care (LTC). Similar to other policies, to claim LTC benefits, the union member must require assistance due to cognitive impairment or be unable to perform 2 or more activities of daily living listed below:
- Bathing
- Eating
- Dressing
- Toileting
- Transferring
- Continence
Read: How are activities of daily living defined in LTC policies?
Are Spouses Covered Under Union Long-Term Care Insurance?
If you are the spouse of a current (or retired) union memory, you may be eligible for LTC insurance coverage as well, depending on the wording of the policy. Under some union LTC policies, spouses of active or retired union members may be eligible to receive LTC benefits. Typical conditions under such union LTC policies include meeting the following requirements:
- The spouse becomes eligible for the coverage at the same time as the insured (or when they become your spouse) starts receiving LTC benefits, provided he/she is not eligible for a Basic Daily Benefit claim at that time.
- Spouse’s eligibility ends when the insured’s eligibility ends, except in the case of the insured’s death while in benefit.
- Spouse’s eligibility is extended for 2 years commencing on the insured’s death, provided they (the insured) was receiving LTC benefits on the date of their death.
If you are an active or retired union member or spouse, you might be eligible for LTC benefits.
Roger R. Foisy & Associates can help you navigate your long-term care insurance claim if it has been denied or terminated. Call us at (905) 286-0050 or fill out the form on this page.
Related Content
Merry Christmas and Happy New Year!
The team at Foisy & Associates wishes you and your loved ones Merry Christmas and a Happy New Year! We hope your holiday season is filled with joy, laughter, happiness, and relaxation. As we look forward to 2022, our team remains committed to providing every client with a very personal level of attention and maximizing their disability and personal injury settlements.
Holiday Hours:
December 24th: Closed at 1 pm
December 27th-28th: Closed
December 31st: Closed at 1 pm
January 3rd: Closed
Foisy & Associates continues to support the Brain Injury Association of Peel and Halton (BIAPH). BIAPH is a non-profit organization that exists for the needs of families and survivors of brain injury in the Peel and Halton Regions. BIAPH facilitates measures to promote the prevention of brain injury, improve quality/care of life, provide community education, and conduct resource searches on behalf of members.
This December, our firm is also holding a toiletry drive and will donate several toiletry kits to the Elizabeth Fry Society of Peel-Halton and St. Leonard’s Place Peel.
Why It’s Important for Personal Injury Lawyers to Monitor Client Social Media
Social media evidence is now commonly used in personal injury cases, with defendants and insurance companies increasing their monitoring of plaintiff accounts. As a lawyer, you need to know what your clients post to their profiles because what may seem like a harmless post can have dire consequences on your file.
There are several examples of courts in the U.S. and Canada allowing social media posts to be admitted as evidence in personal injury cases. In some cases, these posts have had a direct impact on the outcome of the settlement value.
In Sedie v. US, a California personal injury case, social media evidence in conjunction with medical evidence was used to discredit the severity of the plaintiff’s injury. This led to the court concluding that the damages sought by the plaintiff were inflated.
In an Ontario personal injury case, Moretto v Nicolini-Femia, social media evidence was used to reduce the plaintiff’s damages in the assessment of her general damages.
You can read more case law on social media evidence in personal injury cases in the U.S. and Canada here.
The examples above demonstrate the role social media evidence can play in helping insurance companies discover or discredit a plaintiff’s claim about the extent of their injuries.
Clients suffering from injury or disability generally post positive content on their profiles that are only snapshots in time. This content rarely reflects the severity of a person’s pain and suffering. If lawyers are aware of what their clients are posting, during proceedings, they will be able to provide context so evidence can be based on the entirety of the facts and not simply on a single social media post.
Benefits of Monitoring Client Social Media
Increase Value of Files: Building a social media report that paints a picture of your clients’ life before and after their injury or disability can be instrumental in maximizing the value of their claim.
Avoid Bad Clients: You can use social media to determine if a prospective client is telling you the entire story and if they are indeed a file you want to invest in.
Reduce Client Risk: Social media is a rare outlet for clients that are suffering from an injury or illness. However, their posts may be misrepresented in court. Our team’s experience is that once clients become aware that their social media accounts are being monitored, we have noticed an immediate and significant decrease in their social media activity.
How Can Lawyers Monitor Client Social Media?
With more case law emerging that confirms the detrimental effect of social media usage on clients’ settlement values, lawyers can no longer ignore their clients’ activity.
Instead of spending several hours every week manually going through clients’ social media accounts to generate reports, lawyers and paralegals can now rely upon sophisticated tools that save time and increase the value of their files.
At Foisy and Associates, we use Private Footprint. This powerful tool allows our lawyers and paralegals to quickly view, organize, and make sense of the overwhelming volume of social media content generated by clients. Our team easily monitors social media activity for each client separately, flag specific posts, and quickly generate detailed reports that document the lives of our clients before and after life-altering events such as a personal injury or disability.
If you have sustained a personal injury or disability, please contact Foisy and Associates for a free consultation.
Long-Term Care Benefits Denied by Insurance Company
Jason purchased long-term care insurance 20 years ago to alleviate his children from the burden of long-term care costs and ensure he was taken care of in his senior years if the need arose.
Jason paid his insurance premiums religiously, but when he became ill and required ongoing assistance, Jason’s (now adult) children assisted him in filing a long-term care insurance claim. They were shocked when Jason’s benefits were denied by the insurance company.
Jason and his children are not alone; this is a scenario repeating itself all too often and is becoming a significant concern for long-term care insurance policy holders.
It may appear that insurance companies have been surprised by the escalating cost of long-term care and have been doing everything in their power to reduce their losses. In fact, a major Canadian insurance provider recently stopped offering long-term care insurance altogether, while others have significantly reduced benefits and increased premiums.
When Can Insurance Companies Deny Long-Term Care Claims
In Jason’s and most long-term care policies, a person is considered dependent if:
- They cannot perform two or more duties of daily living without substantial assistance.
- Require constant supervision due to cognitive impairment to protect themselves for their safety and health.
An insurance company will deny your claim if you fail to meet their definition of dependent. You need to understand how activities of daily living and cognitive impairment are defined and if you are in fact meeting the criteria listed in the policy.
Read: How are activities of daily living defined in long-term care policies?
Jason moved in with his son because he required assistance in performing activities of daily living. However, the insurance company denied his claim, stating he was able to perform the said activities.
There are strict limitations periods in contractual agreements between parties where the limitation period could be one year or more. If there is no mention of a limitation period, the Ontario Limitations Act, 2002, provides the limitation period which is usually two years from the date of denial of the long-term care claim.
Since there was no mention of a limitation period in Jason’s long-term care insurance contract, he and/or his family must commence legal action within two years of the denial of Jason’s claim for long-term care.
At the point of denial, it would be beneficial to contact a lawyer and seek representation in the case against the insurance company. In Jason’s case, he requires stand-by assistance from another person (his son) to safely perform two or more of the activities of daily living, as described in his policy. This appears to fit the criteria of physical dependency, and Jason may be successful in challenging the denial with the help of a lawyer experienced in disputing and litigating long-term care insurance denials.
Legal representation is also essential when challenging long-term care policy denials based on an insurance company’s interpretation of cognitive impairment which we will discuss in a future blog.
Read: How is cognitive impairment commonly defined in long-term care policies?
If your long-term care insurance claim has been denied or terminated, contact Roger R. Foisy & Associates for a free consultation. Call us at (905) 286-0050 or fill out the form on this page.
Has Your Long Term Disability Been Terminated [Video]?
You have seen little if any improvement in your physical and mental health, but your long term disability has been terminated. You have not received the go-ahead from your doctor to return to work, and you continue to take the same or more medication.
So, how can the insurance company doctor who barely knows you or saw you only once, decide that you can go back to work?
Ask yourself what changed…Why did the insurance company terminate your benefits?
What changed was the definition your insurance company now uses to define disability and your ability to return to work.
If you were told that a diagnosis is required to be eligible for long term disability, let me assure you that this is not true.
Watch our short video that explains why you should contact a lawyer if your long term disability claim has been terminated.
Foisy and Associates personal injury and disability law firm represents individuals who have had their long term disability claims terminated. We have been handling long term disability terminations for more than 20 years, and have a track record of success.
If you face a situation where your long term disability claim has been terminated, contact us and speak to one of our lawyers.
We can help get you the benefits you deserve!
Has Your Long Term Disability Claim Been Denied [Video]?
Your long term disability claim has been denied, and your insurer has offered you to appeal its decision. At this point, you need to pause and think for a moment…what are the chances that the same insurance company that denied your claim will overturn its own decision?
I’ve been a long term disability lawyer for 20 years and have rarely seen an insurance company overturn its denial, and even in those cases, it was usually due to an administrative error.
If your claim was denied, time is running out to file a lawsuit against your insurance company. Your chance of a successful resolution increases ten-fold if you let our offices work with you as soon as you experience an initial denial.
Let us assist in managing your file, and let us communicate with your insurance company. After reviewing and critiquing your insurance company’s file, we can determine if the denial was valid.
Watch our short video that explains why you should contact a lawyer if your long term disability claim has been denied.
Foisy and Associates personal injury and disability law firm represents individuals who have had their long term disability claims denied. We have been handling long term disability denials for more than 20 years, and have a track record of success.
If you face a situation where your long term disability claim has been denied, contact us and speak to one of our lawyers.
We can help get you the benefits you deserve!
Injured from a Fall Due to Ice or Snow? You Must Act Very Quickly!
As of January 29, 2021 Ontario’s Occupiers’ Liability Act was amended to add a requirement of written notice for claims arising from injuries caused by snow and ice.
If you’ve been injured from a fall due to snow or ice in Ontario, you have ONLY 10 DAYS to provide written notice by registered mail to the Municipality if the fall occurred on a municipal sidewalk or roadway. For all other properties, you have ONLY 60 DAYS to provide written notice by registered mail to the property owner or responsible maintenance contractor.
Action Against Ontario Municipalities
The Municipal Act states that no action shall be brought for the recovery of damages against a municipality unless written notice of the claim and of the injury has been hand-delivered or sent by registered mail to the municipal clerk’s office within 10 days after the occurrence of the injury.
Failure to give notice may not prevent you from taking legal action but only if a judge finds that there is reasonable excuse for the insufficient notice and that the municipality is not disadvantaged in responding to your claim. This places the onus on you to prove and may be a difficult threshold to meet. Therefore, we strongly recommend that you adhere to the 10 days’ notice requirements mentioned above.
Action Against Property Owners and Maintenance Contractors
Under the new Section 6.1 of the Occupiers’ Liability Act, no action shall be brought for the recovery of damages for personal injury caused by snow or ice against an occupier or a maintenance contractor retained to remove snow and ice unless written notice of the claim (including the date, time and location of the occurrence) is provided within 60 days after the occurrence of the injury, except in the case of death of the injured person as a result of the injury.
Written notice is to be hand-delivered or sent by registered mail to at least one of the occupiers of the premises, or the independent contractors employed to remove snow or ice on the premises.
As with municipalities, failure to give notice may not prevent you from taking legal action but only if a judge finds that there is reasonable excuse for the insufficient notice and that the occupier and/or the independent maintenance contactor is not disadvantaged in responding to your claim. This once again places the onus on you to prove and may be a difficult threshold to meet. Therefore, we strongly recommend that you adhere to the 60 days’ notice requirements mentioned above.
If you’ve been injured in Ontario from a slip, trip, and fall due snow or ice, you must act quickly. contact us and speak to one of our lawyers.
We can help you get the settlement you deserve!
Long Term Disability and Psychological Distress [Video]
People who are suffering from mental health issues tend to blame their workplace and employer for psychological distress. Focusing on your employer can undermine your long-term disability case because your insurer will just ask you to change where you work.
You are dealing with more than just the general stress of life. These could be issues that are happening in the world, in your home, in your personal life or a health issue such as chronic pain.
Watch our short video that explains the link between phycological distress and long term disability.
Foisy and Associates Personal Injury and Disability Law Firm represents people who are suffering from psychological distress. We have been handling long term disability claims for more than 20 years, and have a track record of success.
If your psychological distress is impacting your ability to work, contact us and speak to one of our lawyers.
We can help you get the benefits you deserve!
Merry Christmas and Happy New Year!
The holiday season is here and it’s time to reflect on the year that has been. No one could have predicted the difficulties 2020 would bring and the challenges it created for everyone. This year we want to extend our holiday greetings to not only our clients but also to frontline workers who are risking their lives in the fight against COVID-19.
We hope your holiday season is filled with joy, laughter, good food, and time reflecting on all the reasons to be optimistic. From the entire team at Foisy & Associates, Merry Christmas and a Happy New Year!
Holiday Hours
December 16th: Closed at 12 PM for staff virtual event
December 24th: Closed at 1 PM
December 25th – 27th: Closed
December 31st: Closed at 1 PM
January 1st: Closed
The team at Foisy & Associates continues to support the Brain Injury Association of Peel and Halton (BIAPH). BIAPH is a non-profit organization that exists for the needs of families and survivors of brain injury in the Peel and Halton Regions. BIAPH facilitates measures to promote the prevention of brain injury, improve quality/care of life, provide community education, and conduct resource searches on behalf of members.
Long Term Disability and Chronic Pain
We tend to recognize pain as only physical, but pain has biological, psychological, and emotional factors and if left untreated or misdiagnosed, there is a possibility it becomes chronic. Diagnosing chronic pain can be difficult as most of the time symptoms cannot be seen, even though the pain is real.
To see if you are suffering from chronic pain you need to ask yourself the following questions:
- Have you been in pain for more than six months?
- Are you dependent on your physician for care?
- Do you find yourself disengaged from work, recreational activities, and feeling increasingly isolated?
If you are experiencing any of the above, chronic pain might be to blame.
While it has taken several years to get there, the Supreme Court of Canada has recognized chronic pain as a disability.
Watch our short video that explains how you can qualify for long term benefits if you suffer from chronic pain.
Foisy and Associates personal injury and disability law firm represents individuals who are suffering from chronic pain. We have been handling long term disability claims for more than 20 years, and have a track record of success.
If you are facing a situation where your chronic pain was not recognized as a disability, contact us and speak to one of our lawyers.
We can help get you the benefits you deserve!
Virtual BIAPH Health Advocates Education Conference on October 28
The second Brian Injury Association of Peel and Halton (BIAPH) Health Advocates Education Conference will be held virtually on October 28, 2020. The theme for this year’s conference is What You’re Missing: Practical Tips and Strategies from Industrial Professionals. This event is the largest Virtual Health Advocates Education Conference in Ontario.
BIAPH’s innovative virtual platform will deliver our trademark rapid podium speakers. Delegates will have full access to all exhibitors and will be able to interact with them online through the platform.
Roger R Foisy who has served as BIAPH President since September 2019 has returned as conference chair and looks forward to holding the best conference of its kind in Canada.
We invite you to watch the lighthearted video below for more information about the conference!
The conference presents an opportunity to promote your organization and reach out to a wide variety of health care and rehabilitation professionals and advocates. Sponsorships have been in high demand.
We look forward to you attending this unique learning experience which will use a multidisciplinary approach to bridge gaps in knowledge and provide practical tips and strategies on how to effectively advocate for clients and assist in ensuring that funding for treatment is provided.
BIAPH is a non-profit organization that exists for the needs of families and survivors of brain injury in the Peel and Halton Regions. BIAPH facilitates measures to promote the prevention of brain injury, improve quality/care of life, provide community education, and conduct resource searches on behalf of members.
If you want to register for the conference or have any questions, please email conference@biaph.com
Here’s What You Should Do If You Receive Your Two-Year LTD Termination Letter
You’ve been receiving long term disability (LTD) benefits and have just received a letter from your insurance company stating that your benefits will be terminated at the two-year mark. The insurance company has sent you this letter because how total disability is defined in your policy changes at the two-year mark. The “two-year mark” refers to the two years after you became totally disabled from working in your occupation. Before you decide to take any action, it’s important to understand the definition of total disability before and after the two-year mark.
Before the “Two-Year Mark”: You cannot perform the essential duties of your own occupation (It does not matter where you are employed, rather the policy only looks at if you can do your occupation).
After the “Two-Year Mark”: For most policies the definition changes from being unable to perform your own occupation to being unable to perform the essential duties of ANY occupation for which you have the education, experience, and/or training. In some insurance policies, there may be a clause that further defines total disability to include your being unable earn a certain percentage of the gross income you were earning at the time of you became disabled.
Coming back to the letter you have just received from the insurance company a few months (typically 3-6 months) before the end of the two-year mark. This means the insurance company has determined that you do not fit under the second definition of total disability (“After the ‘Two-Year Mark’”). In other words, the insurance company believes that even if you cannot do your own occupation, you can work in a different occupation. As a result, you have received an advance warning that your benefits will stop at the two-year mark, or you might have received your benefits till the end of the two-year mark.
Let’s take a look at scenarios that will help better explain this.
Scenario 1
Mark, a construction worker injured his knee on the job and the insurance company agreed he was disabled from his occupation as a construction worker because he could no longer lift heavy objects as he did before. At the two-year mark, the insurance company has now determined that Mark can work in a different occupation (e.g. a desk job), therefore he no longer fits the definition of total disability because the definition of disability changed after the two-year mark. But, a deeper look into this case reveals that Mark is unable to perform a desk job because he does not have the training, experience, or education that is required.
In Mark’s policy, there isn’t a percentage of income earned parameter and even if the insurance company does a transferable skills analysis and determines he can work as a greeter at a retail store, case law suggests that the amount of money he earns in the new occupation should be somewhat commensurate with what he was earning in his original occupation before his disability.
Therefore, given Mark’s training and anticipated pay as a greeter he may still be eligible to receive LTD benefits beyond the two-year mark.
Scenario 2
Jane, is an advertising director for a large marketing company. Regrettably, she has been suffering from anxiety and depression which stems from family, financial, and other past mental and behavioural issues which have recently resurfaced. Her workplace has been somewhat of a poisonous work environment for a number of years. Almost 2 years ago, she stopped working when she could no longer continue working in this unhealthy work environment.
Six months before the two-year mark, Jane’s LTD insurance company advises her that she no longer meets the two-year change of definition. In other words, the insurance company believes that her education, experience and/or training will allow her to continue working in another occupation and possibly in a less poisonous working environment.
In Jane’s policy, there is a specific definition of total disability which states that Jane will be considered totally disabled if she is unable to earn at least 66.67% of her gross income at time she becomes disabled. Based on her gross income of $120,000 per year, the suggested work positions by Jane’s LTD insurance company are occupations that are more likely to pay her $40,000 to $50,000 per year and not the $80,000 per year (as stipulated in the LTD policy).
Therefore, Jane’s ability to continue to earn LTD benefits, even after deducting her wages from some other form of employment, allows her to continue to receive LTD benefits beyond the two-year mark.
When to Contact A Lawyer?
You should be contacting a lawyer as soon as you receive the denial letter, the two-year mark letter, or the change of definition letter from the insurance company. This will let the lawyer review your case at an early stage and determine whether to disagree or agree with the insurance company’s position. In most cases, the insurance company does have the evidence to substantiate its decision to terminate your LTD. Contacting a lawyer at this stage will also give them the lead time required to request and review your file, along with providing a preliminary opinion. So, when the cut-off date for your benefits arrives, your lawyer is in a position to start litigating or commencing an action against the insurance company. Waiting to contact a lawyer until after the cut-off day will cause even further delay in your ability to collect benefits as the lawyer will require time to request, receive and review your file from the insurance company as well as your health care providers.
For your convenience, we have provided answers to the most commonly asked LTD questions. If your LTD has been denied or terminated contact us for a free consultation.
Congratulations to Daniel Berman on his Call to the Bar!
The team at Roger R. Foisy injury law firm is pleased to announce that Daniel Berman, part of our staff since 2018, was recently called to the bar.
Being called to the bar is a milestone in a lawyer’s career, and we couldn’t be happier for Daniel on this achievement. Daniel has already started the transition from student to a member of our injury and disability litigation law team following his successful completion of the bar, and we look forward to his continued growth with us.
Congratulations to Daniel from all of us at the Roger R Foisy injury law firm!
Roger R. Foisy and Associates are Ontario Personal Injury Lawyers with extensive experience in personal injury, long-term disability, and brain injury. Please contact us for immediate support and a free consultation.
Click here to watch our video series about personal injury and personal injury law.
More from Roger R. Foisy:
Can you Claim LTD Because of COVID-19?
Social Media and Personal Injury Law: Can Social Media Affect Your Case?
Can You Claim LTD Because of COVID-19?
The COVID-19 pandemic has changed our way of life and the direct and indirect psychological, social, and economic effects of COVID-19 could affect mental and physical health now and into the future.
Studies have shown that large-scale disasters, whether traumatic, natural, or environmental are almost always accompanied by increase in depression, PTSD, substance use disorder, and a broad range of other mental and behavioural disorders.
COVID-19 is unique from other traumatic events because the government issued lockdown and social distancing protocols affect every person in society, not just those in direct proximity to the virus or in quarantine.
Many of us have lost our jobs while others have had to cope with stress and anxiety while working on the front lines or from home. Some of us have been exposed to the virus, either contracting it, having their loved ones falling sick, and in the worst scenario passing away.
If you are an already fragile person, the stress, anxiety, and PTSD brought on by COVID-19 may lead to your mental health deteriorating. You may no longer be able to work and can be eligible for long term disability (LTD) insurance. When applying for LTD it is important to consider that in most claims the cause of your mental health condition is not relevant.
To better understand the link between LTD and COVID-19, let us explore some scenarios.
Scenario 1: Single Parent Whose Income and/or Bonuses Have Been Cut Due to COVID-19
You are a single parent who was working a mid-level 9-5 job and was living paycheque to paycheque. Due to COVID-19, you had to take a pay cut and/or your yearly bonus was eliminated. This sudden decrease in income which you previously depended on is no longer available to you and is the reason your stress levels have increased drastically. While you were barely keeping it together before, this added stress is the straw that broke the camel’s back. Under this scenario, you are unable to continue work and could be eligible for LTD.
Scenario 2: Loved One Infected With/ Passes Away Due to COVID-19
You experience tremendous stress when your relatives or friends’ contract COVID-19 or fear that they might become infected with the virus. You research and learn about the worst outcomes associated with the virus, which leads to your mental health being impacted. Even worse, you have had a loved one pass away due to COVID-19 and you were unable to be by their side. You feel immense guilt and are unable to move beyond it. Such scenarios can lead to mental health breakdowns and have a direct impact on a person’s ability to work.
Scenario 3: You Work Close to Others
You work in a job that requires you to be close to others and all the information you have received regarding COVID-19 says you should stay at least 6-feet apart from someone else. There is trauma caused by the fear of your existing environment and this will not allow you to work anywhere else.
Scenario 4: Mental Health Deteriorates Due to Unavailability of Treatment
With psychological trauma, if you get treatment quickly you can develop strategies to cope with it. However, with COVID-19, there is a lack of psychiatric or psychological treatment available as some doctors and facilities have closed their offices and are not seeing new patients. There are options available for telephone and videoconferencing, but you are not comfortable with this and want to wait to see a medical professional in-person. The limited options available at this time for your treatment can lead to your mental health becoming worse and increase your inability to work.
The nature and response measures as a result of the ongoing COVID-19 pandemic are unprecedented in modern history. Not only does COVID-19 impact those in close proximity to the virus, but the economic lockdown and social distancing protocols affect every single person in a variety of ways. What is clear is that COVID-19 will have a profound effect on all aspects of society, including mental and physical health.
For your convenience, we have provided answers to the most commonly asked LTD questions. If your LTD has been denied or terminated contact us for a free consultation.
We Are Open and Available to Help
We are available for new consultations during the COVID-19 crisis. Please contact us regarding your Personal Injury or Disability Claim. While our physical offices are closed, our staff is fully functional and working remotely.
To contact us, please call us at 905.286.0050 / toll-free 877.286.0050, or email us at info@injurylawyercanada.com.
We will follow up with you within 2 hours of your call or voice mail that is received during the regular business hours of 9 AM to 5 PM, Monday to Friday, and schedule a call or video conference to discuss your situation. By special appointment we can also schedule an appointment later in the evening or on the weekend.
We look forward to speaking with you soon.
The Roger Foisy Team
Merry Christmas and Happy New Year!
It’s the most wonderful time of the year! A very Merry Christmas to you and your loved ones from the team at Roger R Foisy! We hope you have a wonderful holiday season filled with joy and relaxation, and we wish you health and happiness in 2020.
Our Holiday Hours
- December 24th: Closed at noon
- December 25-27: Closed
- December 31: Closed at noon
- January 1: Closed
 A Season of Giving
A Season of Giving
Leading up to Christmas, we seek to support organizations that make a positive change in our communities.
- We attended the Brain Injury Association of Peel and Halton’s (BIAPH’s) Holiday Party in support of BIAPH’s programs, which helps youth and adults impacted by brain injury.
- We provide care packages to families in need in our community.
Season’s Greetings from Roger R Foisy & Associates to you and your family. Stay safe this Christmas season!
Learn about personal injury from Roger R Foisy:
Personal Injury Potential Settlement Values: Knee Injuries
Knee injuries can occur with little impact and are often the result of a slip and fall or a minor motor vehicle accident.
In this article, we will take a look at four knee injuries and historical examples of the personal injury settlement values victims have received:
- ACL Tear
- Dislocation of the Knee Joint – Lateral View
- Meniscus Tear
- Comminuted Fracture of the Patella
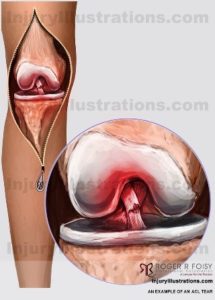 ACL Tear
ACL Tear
An Anterior Cruciate Ligament (ACL) tear is one of the most common knee injuries, especially in athletes that play high demand sports (IE. soccer, football, basketball). ACL tears can be caused by changing direction rapidly, stopping suddenly, slowing down while running or landing from a jump incorrectly. Symptoms include: pain with swelling, loss of full range of motion, tenderness along the joint line, and discomfort while walking.
In 1986, the Court in Papamonolopoulos v Board of Education for the City of Toronto, 56 OR (2d) 1 awarded the injured person $40,000 for injuries that included a torn ACL.
To read the full decision on CanLII, click here.
 Dislocation of the Knee Joint – Lateral View
Dislocation of the Knee Joint – Lateral View
A dislocation of the knee joint happens when bones of the leg are moved in relation to the bone in the thigh. Knee dislocations usually happen after major trauma, such as falls or motor vehicle accidents. Common symptoms include: pain, no feeling below the knee, deformity of the knee, and swelling of the knee.
In 1992, the Court in Moody v Windsor, [1992] BCWLD 405 awarded the injured person $85,000 for injuries that included a dislocated knee.
To read the full decision on CanLII, click here.
 Meniscus Tear
Meniscus Tear
The meniscus is the rubbery, C-shaped disc on your knee. A meniscus tear is a common knee injury often caused by twisting or turning quickly with the foot planted and the knee bent. Meniscus tears can also be caused when lifting something heavy. Common symptoms include knee pain, swelling, stiffness in the knee, and popping or locking of the knee.
In 2004, the Court in Ouellette v Hearst (Corp. of the Town), [2004] OJ No 1120 (QL) awarded the injured person $110,000 for injuries that included a meniscus tear.
To read the full decision on CanLII, click here.
Comminuted Fracture of the Patella
The patella is a small bone located at the front of the knee that protects the knee and connects the front thigh muscles to the tibia (upper part of the leg). Comminuted fractures of the patella are commonly called by a direct blow, such as from a motor vehicle accident or a fall. Common symptoms include pain and swelling in the front of the knee, bruising, and an inability to straighten the knee or walk.
In 2005, the Court in Mason v Moore, [2005] OJ No 3799 awarded the injured person $90,000 for injuries that included a fracture of the patella.
To read the full decision on CanLII, click here.
Receiving the Settlement You Deserve
People often believe that settlement value is mostly determined by the extent of the injury. While this is a factor, the most important information is how the injury has impacted your life. In other words, what does the injury prevent you from being able to do and how does this affect you?
I encourage you to view my previous article about seeking compensation for leg injuries, wherein I discuss, in greater detail, the injury and how victims can receive the compensation they deserve.
A thorough lawyer should take the time to fully understand your specific situation, including your life and responsibilities before and after your accident, to ensure you do not under-settle your case. By quantifying every possible loss, you are more likely to receive a just settlement that will help to ease the financial burdens that usually occur during recovery.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
*Roger R. Foisy is not a medical professional. The advice in this blog is not meant to be a substitute for medical advice.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
Personal Injury Potential Settlement Values: Leg and Ankle Injuries
Lower extremity (leg, knee and ankle) injuries tend to occur over a wide range of unfortunate accidents. As a general rule, less impact is required for knee and ankle injuries which can result from a slip and fall or a less impactful motor vehicle accident. In contrast, the femur (thigh) – which is the longest, heaviest, and strongest bone in the human body – tends to sustain injury from more serious motor vehicle accidents involving greater force of impact.
In this article, we will take a look at six leg and ankle injuries and historical examples of the personal injury settlement values victims have received:
- Tibial Shaft Fracture
- Lateral Malleolus Fracture
- Bimalleolar Fracture
- Medial Malleolus Fracture
- Fracture of the Distal Fibula Along the Medical Cortex Above the Level of the Fibial Plateau
- Fracture of the Lateral Tibial Plateau
 Tibial Shaft Fracture
Tibial Shaft Fracture
A fracture that occurs to the long bone that runs below the knee and above the ankle (tibia). Tibial shaft fractures are often caused by high-energy collisions, such as motor vehicle accidents and falling while playing sports such as skiing or soccer. Common symptoms include: pain, inability to walk or put weight on the leg, the bone protruding through a break in the skin, or a loss of feeling in the foot.
In 2012, the Court in Riehl v Hamilton (City), 2012 ONSC 3333 awarded the injured person $75,000 for injuries that included a tibial shaft fracture.
To read the full decision on CanLII, click here.
 Lateral Malleolus Fracture
Lateral Malleolus Fracture
A fracture to the bone located to the outer aspect of the ankle. Lateral malleolus fractures are commonly caused by a roll of the ankle, an awkward landing from a jump, or a directly blow to the outer ankle. Common symptoms include: sharp outer ankle or lower leg pain, swelling, and bruising.
In 2002, the Court in Hutchison v Dalton, [2002] OJ No 4764 awarded the injured person $50,000 for injuries that included a lateral malleolus fracture.
To read the full decision on CanLII, click here.
 Bimalleolar Fracture
Bimalleolar Fracture
A bimalleolar fracture is the result of a fracture to the two lower bones that make up the ankle: one on the outside of the ankle and one on the inside. Bimalleolar fractures are often caused by motor vehicle accidents, falls, and twisting the ankle. Common symptoms include: swelling, tenderness, bruising, and inability to bear weight.
In 2011, the Court in Druet v Sandman Hotels, 2011 BCSC 232 awarded the injured person $55,000 for injuries that included a bimalleolar fracture.
To read the full decision on CanLII, click here.
 Medial Malleolus Fracture
Medial Malleolus Fracture
A medial malleolus fracture is the result of a break in the bony process located at the inner part of the ankle (medial malleolus). These fractures can be caused by a rolled ankle, an awkward landing from a jump, or a fall. Common symptoms include: sharp inner ankle pain, lower leg pain, swelling, and bruising.
In 2002, the Court in Hutchison v Dalton, [2002] OJ No 4764 awarded the injured person $50,000 for injuries that included a medial malleolus fracture.
To read the full decision on CanLII, click here.
 Fracture of the Distal Fibula Along the Medical Cortex Above the Level of the Fibial Plateau
Fracture of the Distal Fibula Along the Medical Cortex Above the Level of the Fibial Plateau
As one of the more common fractures at the ankle, distal fibula fractures are often the result of an inversion injury. Distal fibula fractures are often caused by trauma and the ankle twisting inward or outward. Common symptoms include: severe ankle pain, swelling, bruising, and an inability to bear weight.
In 2009, the Court in Rizzolo v Brett, 2009 BCSC 732 awarded the injured person $125,000 for injuries that included a fracture of a distal fibula.
To read the full decision on CanLII, click here.
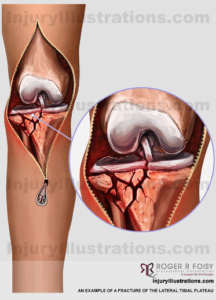 Fracture of the Lateral Tibial Plateau
Fracture of the Lateral Tibial Plateau
A tibial plateau fracture is the result of a break in the proximal part of the shinbone. Tibial plateau fractures can be caused by motor vehicle accidents, falls, or sports injuries. Common symptoms include: swelling, bruising, and an inability to bear weight.
In 2012, the Court in Riehl v Hamilton (City), 2012 ONSC 3333 awarded the injured person $75,000 for injuries that included a fracture of the lateral tibial plateau.
To read the full decision on CanLII, click here.
Receiving the Settlement You Deserve
People often believe that settlement value is mostly determined by the extent of the injury. While this is a factor, the most important information is how the injury has impacted your life. In other words, what does the injury prevent you from being able to do and how does this affect you?
I encourage you to view my previous article about seeking compensation for leg and knee injuries, wherein I discuss, in greater detail, the injury and how victims can receive the compensation they deserve.
A thorough lawyer should take the time to fully understand your specific situation, including your life and responsibilities before and after your accident, to ensure you do not under-settle your case. By quantifying every possible loss, you are more likely to receive a just settlement that will help to ease the financial burdens that usually occur during recovery.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
*Roger R. Foisy is not a medical professional. The advice in this blog is not meant to be a substitute for medical advice.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
Personal Injury Potential Settlement Values: Hip and Pelvis Injuries
Hip and pelvis injuries were once a common result of motor vehicle accidents. But with advanced safety features including lower console and lower door side airbags, these injuries have been greatly reduced. However they remain a prominent outcome of slip/trip and fall accidents, particularly for the elderly.
In this article, we will take a look at hip and pelvis injuries and historical examples of the personal injury settlement values victims have received:
- Intertrochanteric Fracture
- Labral Tear of the Hip
- Right Superior Fracture of the Inferior Pubic Rami
Intertrochanteric Fracture
A fracture in the hip region often caused by a hard fall. These fractures are most common in individuals above 80 years of age. Common symptoms include: the leg feeling shortened, externally rotated, and/or groin pain with leg movement.
In 2014, the Court in Manzoor Ur-Rahman v Oma Devi Mahatoo et al, 2014 ONSC 2636 awarded the injured person $90,000 for injuries that included an intertrochanteric fracture.
To read the full decision on CanLII, click here.
 Labral Tear of the Hip
Labral Tear of the Hip
The labrum is a rim of soft tissue surrounding the hip socket that adds to the stability of the hip. Common symptoms of a labral tear of the hip include: pain in the groin or front of the hip, locking, clicking or a catching sensation in the hip. Hip labral tears are generally caused by trauma (IE. car accident), structural abnormalities, and repetitive motions (IE. twisting in golf).
In 2012, the Court in Macdonald v Hazel, 2012 BCSC 2079 awarded the injured person $80,000 for injuries that included a labral tear of the hip.
To read the full decision on CanLII, click here.
Right Superior Fracture of the Inferior Pubic Rami 
These fractures occur in the pelvic area and are often the result of a direct blow. These fractures often result from a fall from a standing position or in motor vehicle accidents. Common symptoms include: groin pain, leg pain, difficulty walking.
In 1992, the Court in Olah v Goedecke, [1992] BCJ No 2585 awarded the injured person $55,000 for injuries that included a pelvic fracture.
To read the full decision on CanLII, click here.
Receiving the Settlement You Deserve
People often believe that settlement value is mostly determined by the extent of the injury. While this is a factor, the most important information is how the injury has impacted your life. In other words, what does the injury prevent you from being able to do and how does this affect you?
I encourage you to view my previous article about seeking compensation for arm, wrist, and hand injuries, wherein I discuss, in greater detail, the injury and how victims can receive the compensation they deserve.
A thorough lawyer should take the time to fully understand your specific situation, including your life and responsibilities before and after your accident, to ensure you do not under-settle your case. By quantifying every possible loss, you are more likely to receive a just settlement that will help to ease the financial burdens that usually occur during recovery.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
*Roger R. Foisy is not a medical professional. The advice in this blog is not meant to be a substitute for medical advice.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
Personal Injury Potential Settlement Values: Wrist and Hand Injuries
In our previous article, we discussed arm injuries and how they are often caused by defensive instincts just before impact from a motor vehicle accident. Similarly, wrist and hand injuries are often defensive, and particularly common in slip and fall accidents. In this article, we will take a look at three arm, wrist, and hand injuries and historical examples of the personal injury settlement values victims have received:
 Scaphoid Fracture
Scaphoid Fracture
The scaphoid is one of the eight carpal bones of the wrist. Scaphoid fractures are commonly caused by falls onto an outstretched hand. Symptoms include: Wrist pain, swelling or bruising at the thumb side of the wrist.
In 2013, the Court in Matthew Pierce and Robert Pierce v. City of Hamilton, 2013 ONSC 6485 awarded the injured person $75,000 for injuries that included a scaphoid fracture.
To read the full decision on CanLII, click here.
 Carpal Tunnel Syndrome
Carpal Tunnel Syndrome
Carpal tunnel syndrome results in numbness, tingling, and weakness in the hand as a result of pressure on the median nerve in the wrist. Common symptoms include: numbness or pain in the hand, forearm or wrist; occasional tingling in the hand, occasional pain in the forearm, and stiffness in the fingers.
In 2012, the Court in Shaw v Shaw, 2012 ONSC 590 awarded the injured person $65,000 for injuries that included carpal tunnel syndrome.
To read the full decision on CanLII, click here.
 Partial Tear of the Flexor Tendon of the Fifth Digit
Partial Tear of the Flexor Tendon of the Fifth Digit
A partial tear of the flexor tendon of the fifth digit (the “pinky”) can affect your ability to bend and straighten the fifth digit. Tears can be caused by cuts or sudden pulls against a strong grip. Common symptoms include: inability to bend the fifth digit, pain when fifth digit is bent, and numbness in the fingertip.
In 2003, the Court in Allen v Lawrence Avenue Group Ltd, 2003 CanLII 43571 awarded the injured person $50,000 for injuries that included a tear for the fifth digit.
To read the full decision on CanLII, click here.
Receiving the Settlement You Deserve
People often believe that settlement value is mostly determined by the extent of the injury. While this is a factor, the most important information is how the injury has impacted your life. In other words, what does the injury prevent you from being able to do and how does this affect you?
I encourage you to view my previous article about seeking compensation for arm injuries, wherein I discuss, in greater detail, the injury and how victims can receive the compensation they deserve.
A thorough lawyer should take the time to fully understand your specific situation, including your life and responsibilities before and after your accident, to ensure you do not under-settle your case. By quantifying every possible loss, you are more likely to receive a just settlement that will help to ease the financial burdens that usually occur during recovery.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
*Roger R. Foisy is not a medical professional. The advice in this blog is not meant to be a substitute for medical advice.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
Dress Down for Brain Injury Awareness Month This June
June is Brain Injury Awareness Month. In Canada, approximately 160,000 Canadians suffer brain injuries every year with incidence and reporting rates continuing to rise. The prevalence of brain injury outpaces breast cancer, multiple sclerosis, spinal cord injury, and HIV/AIDS combined, and it remains the number one killer and disabler of people under 44.
Last year, my team and I launched “Dress Down for Brain Injury” to raise awareness and funds in support of Brain Injury Awareness Month. Every Friday, each of us will contribute $5 so we can enjoy wearing casual clothes for the day. At the end of the month, the firm will match those donations 100% and give all proceeds to the Brain Injury Association of Halton Peel.
I encourage you to join us by having your own office take part in Dress Down for Brain Injury Awareness Month, matching whatever amount you are comfortable with to help us support this important and worthwhile cause.
Roger R. Foisy is an experienced Personal Injury Lawyer in Ontario who has helped clients with brain injuries receive compensation. If you or a loved one has suffered a brain injury, please contact us for immediate support and a free consultation.
*Roger R. Foisy has completed courses in Neurorehabilitation, Neurobehavioral Disorders, Advanced Brain Injury Rehabilitation, Cognitive Interventions for Adults with Acquired Brain Injuries, and Neuropsychological Assessments: Beyond Testing from Brock University. However, he is not a medical professional. The advice in this blog is not intended as a substitute for medical advice.
More on Brain Injury from Roger R. Foisy:
Personal Injury Potential Settlement Values: Arm Injuries
Arm injuries are often caused by instinctively holding out ones arm as a defensive action just before accident impact and sometimes due to the impact from air bags deployed at explosive speeds. In this article, we will take a look at four arm injuries and historical examples of the personal injury settlement values victims have received:
- Dislocation of Elbow Joint
- Monteggia Fracture: Anterior Dislocation of the Radial Head with Anterior Angulation of Fractured Ulnar Shaft
- Colles Fracture
- Comminuted Intra-Articular Fracture of the Olecranon
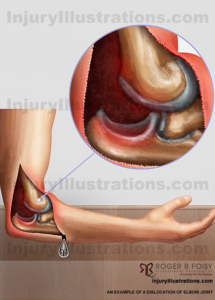
Dislocation of Elbow Joint
A dislocation of the elbow occurs when the bones of the elbow move out of place compared with the bone of the arm. Elbow dislocations are commonly caused by hard falls where the arm is extended completely, as well as motor vehicle accidents. Symptoms include: severe pain in the elbow, swelling, and an inability to bend the arm.
In 2008, the Court in Thorp v Gerow, 2008 BCSC 622 awarded the injured person $50,000 for injuries that included a dislocated elbow.
To read the full decision on CanLII, click here.
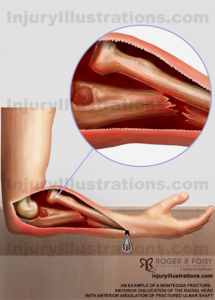
Monteggia Fracture: Anterior Dislocation of the Radial Head with Anterior Angulation of Fractured Ulnar Shaft
A fracture of the forearm involving a dislocation of the radial head and a fracture of the ulna. Monteggia fractures are most commonly caused by falls on an outstretched arm. Symptoms include: arm pain, swelling of the forearm, deformity, swelling of the hand, swelling of the wrist, limited range of motion.
In 1996, the Court in Roy v Benvie, [1996] BCWLD 2293 awarded the injured person $60,000 for injuries that included a monteggia fracture.
To read the full decision on CanLII, click here.

Colles Fracture
A Colles Fracture occurs when the radius bone in your forearm breaks. The radius bone extends from the elbow to the thumb. This fracture is most often caused by an individual falling onto a hard surface while stretching their arms out to break their fall. Common symptoms include: change in the shape or swelling of the forearm right above the wrist, inability to hold or lift heavy objects, and wrist pain.
In 2008, the Court in Guy v Toronto (City), [2008] OJ No 5126 awarded the injured person $30,000 for injuries that included a Colles Fracture.
To read the full decision on CanLII, click here.
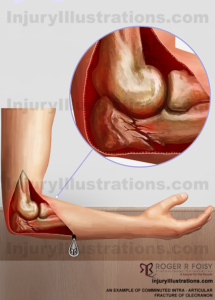 Comminuted Intra-Articular Fracture of the Olecranon
Comminuted Intra-Articular Fracture of the Olecranon
Involves a fracture of the lower portion of the elbow and is often caused by a fall or direct trauma to the elbow, particularly in motor vehicle accidents. Common symptoms include: intense elbow pain, swelling over the bone, inability to straighten the elbow.
In 2004, the Court in Milnes v Burlington, [2004] OJ No 1407 awarded the injured person $30,000 for various injuries that included a fracture of the olecranon.
To read the full decision on CanLII, click here.
Receiving the Settlement You Deserve
People often believe that settlement value is mostly determined by the extent of the injury. While this is a factor, the most important information is how the injury has impacted your life. In other words, what does the injury prevent you from being able to do and how does this affect you?
I encourage you to view my video on how personal injury settlement values are determined wherein I discuss, in greater detail, how victims can receive the compensation they deserve.
A thorough lawyer should take the time to fully understand your specific situation, including your life and responsibilities before and after your accident, to ensure you do not under-settle your case. By quantifying every possible loss, you are more likely to receive a just settlement that will help to ease the financial burdens that usually occur during recovery.
If you have sustained an arm injury or other personal injury at another party’s fault, please do not hesitate to contact me and my team of experienced Ontario personal injury lawyers for a free consultation.
*Roger R. Foisy is not a medical professional. The advice in this blog is not meant to be a substitute for medical advice.
More on Personal Injury from Roger R. Foisy:
Understanding the Lasting Impacts of a Spine Injury
Whether the result of a slip and fall, a serious motor vehicle accident, or another accident, a spine injury can be serious and have profound impacts on a person’s life. Often, the effects extend far beyond the physical injury itself and may have lasting influences on someone’s physical and psychological wellbeing.
In this article, I begin by highlighting six of the most common types of spine injuries before discussing the short and long-term impacts they can have and how these repercussions can affect a personal injury settlement.
Common Spine Injuries
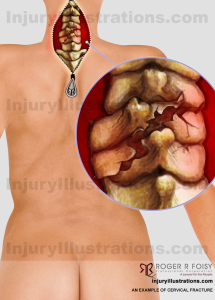 |
 |
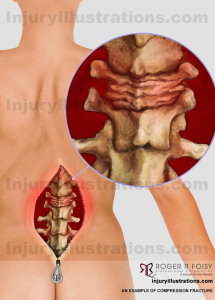 |
Cervical Fracture of the C5/C6Among some of the most devastating injuries, cervical fractures may occur in high-speed motor vehicle accidents with significant head or facial trauma. Cervical fractures to the C5/C6 may cause some or total paralysis of the wrists, hands, trunk, and legs.
Learn more about potential settlement values.
|
Back – Thoracic Compression Fracture – T9These fractures most often occur when the spinal column is subjected to forces that are greater than its strength and stability. Thoracic compression fractures are most often caused by falls from heights, motor vehicle accidents, and penetrating trauma. Common symptoms include: severe back pain, deformity of the spine (i.e. “hunchback”), and some pain relief when lying down.
Learn more about potential settlement values.
|
Back – Compression Fracture of the L1 VertebraeCompression fractures are generally the result of too much pressure on the vertebral body. Compression fractures can be caused by trauma to the spinal vertebrae from falls, jumps, or motor vehicle accidents. Common symptoms include: pain or numbness in the back, legs, and arms.
Learn more about potential settlement values.
|
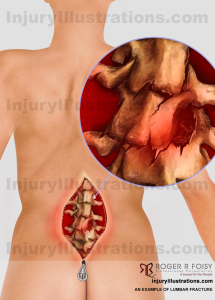 |
 |
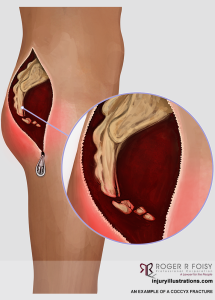 |
Back – Lumbar FractureA lumbar fracture is a fracture in the lower back, where the spine curves inward to the abdomen. Lumbar fractures can be caused by motor vehicle accidents, falls, and sports injuries. Common symptoms include: back pain, tingling, muscle spasms, bowel/bladder changes, and paralysis.
Learn more about potential settlement values.
|
Sacral FractureA sacral fracture is a break of the triangle-shaped bone found at the bottom of the spine. Sacral fractures can be caused by hard falls and motor vehicle accidents. Common symptoms include: lower back, buttock, or hip pain; pain in the front of the thigh and groin; bruising and swelling around the sacral area; and weakness of the lower limbs.
Learn more about potential settlement values.
|
Coccyx FractureA fracture of the coccyx is a fracture of what is commonly referred to as the tailbone. Fractures of the coccyx are often caused by falls onto a seated position or childbirth. Common symptoms include: pain and tenderness in the tailbone area, bruise, and straining and painful bowel movements.
Learn more about potential settlement values.
|
Recovering After a Spine Injury
 One of the challenges associated with injuries of the spine is that people often expect themselves to recover more quickly than they actually do. While the initial spine injury may heal in six to eight weeks, the road to complete recovery is often much longer or unfortunately never attained..
One of the challenges associated with injuries of the spine is that people often expect themselves to recover more quickly than they actually do. While the initial spine injury may heal in six to eight weeks, the road to complete recovery is often much longer or unfortunately never attained..
Beyond the nature of the physical injury itself, other factors that influence recovery include:
- Age: Typically, younger people are able to recover more rapidly than those who are older.
- Lifestyle: Personal circumstances such as needing to return to work or take care of young children may prevent someone from taking the time and space they need to fully recover; therefore prolonging or possibly preventing a full recovery.
- Location: Depending on where a person lives, they may struggle to find good care or may not be able to access it at all.
It’s important to recognize that, especially if the spine injury is the result of a severe motor vehicle accident, the harm may be so great that damage to the spine isn’t the only injury. Any additional injuries may further complicate or extend recovery and need to be taken into account when assessing how injuries have affected a person’s life and the type of supports they will need going forward.
The Long-Term Impacts of a Spine Injury
Chronic Pain
Chronic pain affects up to 70% of patients diagnosed with spine injuries[i] and can include both nociceptive and/or neuropathic pain:
- Nociceptive chronic pain is the more common of the two and includes visceral and musculoskeletal pain like throbbing bone aches, tense muscles, or headaches. It can develop as a response to the initial injury, due to muscle or joint overuse, or a combination of both.
- Neuropathic chronic pain occurs when nerves themselves are damaged. This type of chronic pain can be sporadic or constant and may feel shooting, burning, aching, or numbing. Ultimately, how it manifests varies between individuals.
Appropriate treatment for chronic pain may include medication as well as physiotherapy, psychological counselling, and other services.
Psychological Pain
A majority of people affected by a spine injury also suffer a degree of psychological harm. In some cases, it may be due to how the injury happened. Someone involved in a motor vehicle accident, for example, may find themselves becoming nervous or scared to drive afterwards. Other times psychological pain may be more related to the effects the injury has on someone’s life. If an individual’s injuries prevent them from socializing with friends and family, they could find themselves becoming depressed, while concerns about money could lead to feelings of anxiety.
Managing chronic pain can be a long and multi-disciplinary process. A person’s care team may include pain specialists, spine injury specialists, psychologists, physiotherapists, and other experts, all of whom work together to address physical and psychological sources of persistent pain.
Getting the Right Care Following a Spine Injury
In my experience, I have found that one of the best actions someone with an injury (spine or other) can take is involving an Occupational Therapist in their care early on. Occupational Therapists have a robust understanding of the body and its physical, psychological, and cognitive functions and are focused on identifying tools and strategies that can help patients return to their normal lives.

In assessing individual situations, Occupational Therapists consider holistic questions such as:
- Do a person’s living arrangements enable their recovery? If the home has stairs, for example, will that be a challenge?
- Are there any aids that would further a person’s recovery and rehabilitation like body pillows or an ice pick for a person’s cane?
- How is the individual doing psychologically and cognitively? Would they benefit from a referral to a specialist in pain, psychology, or another area of care?
Occupational Therapists can also help patients work through the concept of hurt versus harm in their day-to-day lives. After a spine injury, many people find that otherwise normal motions like lifting their arms while getting dressed can cause pain. Avoiding these movements altogether can sometimes lead to unintentional consequences down the road like muscle stiffness or fatigue.
This isn’t to say that all pain is good pain, and there are many situations where hurt either does mean or will lead to harm. By working with a rehabilitation specialist like an Occupational Therapist, an individual will be able to better understand their own limitations and learn exercises, activities, and modifications that will advance their recovery without adversely affecting them in the long term.
Working with an Occupational Therapist also benefits those seeking compensation for their injuries. When I recommend an Occupational Therapist to my clients, I get a report that provides me with a comprehensive breakdown of where my client was before the accident, where they ended up because of it, and where they have returned to since. This detailed information gives me the ability to precisely quantify my client’s claims and the damages they have sustained so I can clearly demonstrate how the injury has affected them.
To learn more about Occupational Therapists and the work they do, visit solutionsforliving.ca or function-ability.com. Both provide overviews of some key services as well as articles and other helpful resources.
Receiving the Settlement You Deserve
People often believe that settlement value is mostly determined by the extent of the injury. While this is a factor, the most important information is how the injury has impacted your life. In other words, what does the injury prevent you from being able to do and how does this affect you?
A thorough lawyer should take the time to fully understand your specific situation to ensure you do not under-settle your case. By quantifying every possible loss, you are more likely to receive a just settlement that will help to ease the financial burdens that usually occur during recovery.
If you have sustained a spine injury or other personal injury at another party’s fault, please do not hesitate to contact me and my team of experienced Ontario personal injury lawyers for a free consultation.
*Roger R. Foisy is not a medical professional. The advice in this blog is not meant to be a substitute for medical advice.
More on Personal Injury from Roger R. Foisy:
- How Mild Traumatic Brain Injuries (mTBIs) Affect the Family
- Social Media and Personal Injury Law: Can Social Media Affect Your Case?
- Recognizing the Signs and Symptoms of a Concussion
[i] Finnerup NB. Pain in patients with spinal cord injury. Pain 2013; 154 (Suppl. 1): S71-6.
Merry Christmas and Happy New Year!
On behalf of the Roger R Foisy team, we would like to wish you a Merry Christmas. We hope you are able to enjoy the season in the company of your closest family and friends, and we wish you all the best in the New Year.
Our Holiday Hours
- December 21: Closed at 2:30 pm
- December 24-26: Closed
- December 27-28: Open
- December 31: Closed at 2:30 pm
- January 1: Closed
A Season of Giving
Leading up to Christmas, we have been getting into the giving spirit by contributing to a number of organizations and causes:
- We participated in the CP24/CHUM Christmas Wish Toy Drive.
- We attended the Brain Injury Association of Peel and Halton’s (BIAPH’s) Holiday Party in support of the “Headspin” program, which helps youth and young adults impacted by brain injury.
Our biggest initiative this season, however, has been our staff food drive. As a team, we collected food and packaged it along with gift certificates to help several local families with the extra burdens and expenses that often come with the holidays. The packages were delivered to the families this past week.

Season’s Greetings from Roger R Foisy to you and your family. Stay safe this Christmas season!
Learn about personal injury from Roger R Foisy:
How Past Marijuana Use May Impact Personal injury Claims
Marijuana is the most commonly used drug in North America. Most marijuana users begin experimenting in adolescence, and according to the Canadian Centre on Substance Use and Addiction, over 25% of Canadian youth aged 15-24 use marijuana.1
With the recent legalization of cannabis for recreational use in Canada, I wanted to explore both how marijuana affects the brain and the impact that the past use of marijuana may have on personal injury claims.
How Marijuana Affects the Brain
Although cannabis flowers produce more than 100 types of chemical compounds known as cannabinoids, the two most common are:
- THC (delta-9-tetrahydrocannabinol), the primary psychoactive component.
- CBD(cannabidiol), which is not as psychoactive and is being studied primarily for medicinal applications.
When inhaled or ingested, these chemical compounds enter the blood stream and are carried towards the brain where they bind with cell receptors and change the ways in which cells communicate with each other. This in turn can trigger reactions in regions throughout the brain that influence memory, thinking, concentration, sense, perception, and coordination.
Scientific Studies: The Effects Marijuana May Have on Developing Brains
 According to neuroscientific studies, our brains continue to develop through our early to mid-20s and are sensitive during this time to long-term or lasting harm that can be caused by substances like marijuana. For example, the frontal cortex (the area responsible for memory, judgement, and planning) is one of the last areas to develop and is therefore highly susceptible to permanent damage2:
According to neuroscientific studies, our brains continue to develop through our early to mid-20s and are sensitive during this time to long-term or lasting harm that can be caused by substances like marijuana. For example, the frontal cortex (the area responsible for memory, judgement, and planning) is one of the last areas to develop and is therefore highly susceptible to permanent damage2:
- 43 studies of chronic marijuana users found evidence of brain abnormalities and altered neural activity. After adolescents started to use marijuana structural and functional changes occurred rapidly, and users who started smoking marijuana before the age of 16 were more likely to be impulsive and more susceptible to addiction.3
- In another study, neuroscientists used MRI to look for changes in the brains of individuals aged 18-25 who weren’t dependent but smoked at least once per week. Results showed brain changes that affected motivation, pleasure, and addiction, with participants who smoked more often showing more severe differences.
Scientists skeptical of these studies have argued that most fail to control for the use of alcohol and other societal factors. Others have proposed that genetics could have a greater impact on brain development than marijuana, while other research still has suggested cognitive changes may only be temporary unless used in dangerously high quantities from a very early age.4
Ultimately, while further study is needed into whether slightly frequent or infrequent use of marijuana among adolescents has significant long-term effects, the general consensus is that very frequent use of marijuana from an early age is likely detrimental to brain development.
Could Past Marijuana Use Impact Personal injury Claims?
In accident or injury cases, medical proof is crucial for determining what benefits an injured claimant is entitled to. When medical opinion is attributed to the accident, the claimant is generally entitled to benefits. If marijuana use from adolescence permanently or significantly impacted that person’s brain development, that information could be used to assess whether the injuries were caused by the accident or marijuana use. That result could have a significant effect on the benefits a long-term marijuana user receives if injured in an accident.
It is important emphasize that, as of today, it would be difficult to prove on a medical basis that a claimant’s past use of marijuana plays a significant role in brain development. That could change, however, as more in-depth research is conducted and new evidence emerges.
2 ibid.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
Social Media and Personal Injury Law: Can Social Media Affect Your Case?
Social media plays a prominent and important role in our day-to-day lives—enabling us to share photos we like, post updates about experiences, and catch up with friends and family. But if you have sustained an injury and are involved in a personal injury case, these simple posts and pictures can have major implications.
Today, social media evidence is most commonly used in personal injury, family law, and employment practices. Over half of the lawyers surveyed in one report noted a rise in the last two years in lawsuits related to data, images, and posts made on social media networks and other online platforms.
Here, I take a closer look at this topic and explore the ways in which people are using social media, how it is impacting personal injury law, and some steps plaintiffs can take to keep themselves protected when using social media.
How Canadians Are Using Social Media
Digital technologies, social media included, have become important parts of many people’s lives. Regardless of their age or gender, individuals are posting, sharing, or being tagged—and usage rates are only going up.
In 2017, over 22 million Canadians (64% of the population) were social media users. Ontario accounted for nearly half of that number with 10 million active social media users (67% of the population) across the province. Two-thirds of all social media users in Canada—especially those on Facebook, Instagram, and Snapchat—use the platforms on a daily basis. Facebook remains the most popular platform with 82% of individuals 18-35 and 61% of people over 55 using it regularly.
When we take a closer look at the demographics, we find some compelling trends. Maybe the most interesting among them is that although young people continue to dominate when it comes to the regular engagement with social media, the fastest joining age group is actually older Canadians. Between 2013 and 2016, the number of Canadians between the ages of 65 and 74 using the internet increased 16%, while those 75 and older saw a 15% increase.
 How Social Media Is Impacting Personal Injury Law
How Social Media Is Impacting Personal Injury Law
A decade ago requests for access to plaintiffs’ social media profiles and the court’s willingness to accept social media as evidence would have been exceptions, but today this is rapidly becoming the norm. The case of Ottenhof v Ross (2011), for example, concluded that pages of social media accounts are documents for the purpose of discovery and should be listed in a party’s affidavit of documents if relevant. In Ottenhof, the plaintiff brought an action claiming damages for an assault by the defendant. The defendant discovered the existence of the plaintiff’s Facebook profile and requested access, but the plaintiff refused. In a motion to ‘compel refusal on an examination of discovery’, the judge held that the defendants have permission to cross-examine the plaintiff on the affidavit of documents and that the plaintiff must preserve Facebook contents like any other piece of evidence. In addition, the judge stated that access to a party’s social media account by acquiring his or her password is overly intrusive unless the party claims a level of disability that inhibits use of technology as part of the damages.
Many people might assume that photos and posts hidden behind privacy settings cannot be seen or accessed, but this is not always so. Consider two relevant cases that highlight this:
- Leduc v Roman (2009) held that both public and private social media profiles can be scrutinized for evidence. Although the plaintiff’s pictures were under a private setting, the court ruled that because posted public pictures on Facebook as well as hundreds of her friends had access to her private Facebook content, the plaintiff did not have a serious expectation of privacy. Essentially, if a plaintiff put out evidence publicly on social media, any private information can be cross-examined to learn what relevant content was posted on the profile.
Where, in addition to a publicly-accessible profile, a party maintains a private Facebook profile…it is reasonable to infer from the presence of content on the party’s public profile that similar content likely exists on the private profile. A court then can order the production of relevant posting on the private profile.
– Superior Court Justice David Brown in Leduc v Roman
- Papamichalopoulos v Greenwood (2018) affirmed the upward trend towards the production of private social media material. In Papamichalopoulos v Greenwood, the court ordered the injured plaintiff to turn over social media material despite it being shielded under a privacy setting. The plaintiff had claimed damages for sustained back injuries. However, publicly available Facebook pictures revealed the plaintiff socially active with no signs of pain or discomfort. Citing Leduc, the court argued that it is reasonable to assume that content on a party’s public profile is similar to content in their private profile. Therefore, access to the plaintiff’s private social media was considered reasonable because pictures of the plaintiff before and after the injury can shed light on the extent and legitimacy of the injury.
As these examples illustrate, it has in many ways become standard practice for lawyers to examine the social media profiles of a plaintiff in a personal injury case.
The Role Social Media Can Play in Determining the Extent of Injuries in Personal Injury Cases
In personal injury cases, social media evidence can play a role in helping the defence disprove or discredit a plaintiff’s claim about the extent of their injuries. A few recent cases highlight the importance of social media evidence in the litigation process including:
- A 2007 case, Kourtesis v Joris, in which the court dismissed the plaintiff’s personal injury claims because pictures from her social media account contradicted the extent of her injuries.
- A 2015 case in which a claimant from British Columbia sued for damages resulting from two car accidents that left her depressed and stuck to her house. The plaintiff’s case was dismissed because social media pictures revealed her partying, drinking, and engaging in fun activities that were inconsistent with her claims of emotional and physical trauma.
Despite the above examples, it is important to acknowledge that the courts have treated social media evidence with some skepticism when assessing emotional trauma in particular. Evidence shows that individuals generally post positive content on their social media profiles that does not necessarily accurately represent their life. Certain pictures may only be snapshots in time, which do not reflect the significance of a person’s pain or suffering. Thus, the judge has the discretion to weigh the evidence based on the entirety of the facts and not simply on a single social media post.
Nevertheless, there is always a risk that social media content may sway a jury against a claimant who posted images, statements, or other information online that contradicts their claim.
 How Plaintiffs Can Protect Themselves on Social Media
How Plaintiffs Can Protect Themselves on Social Media
Although you don’t need to avoid social media entirely during your case, it is in your best interest to exercise caution in terms of how, when, and why you use it.
Some tips to keep in mind are:
- Don’t post about your lawsuit or conversations you have had with your lawyer.
- Change your privacy settings to prevent being tagged in photos after the event or ask anyone who has posted any to remove them. Talk with your friends and family as well so they know and understand what your new social media preferences and limitations are.
- Avoid posting, tweeting, sharing photos, or releasing other status updates.
- Never accept a connection request from an individual you neither know nor recognize.
The general rule of thumb is that if you wouldn’t be comfortable sharing it with the defence lawyers, don’t post it.
Based on the exponential increase of social media networks and platforms among Canadians across all ages, personal injury lawyers must ensure that claimants suffering from physical or emotional injuries and who are seeking legal help are prepared for all possible outcomes. More and more this means warning prospective clients of the pitfalls of social media and how it might negatively impact their case.
Approaching a case with detailed preparation and a solid plan will alleviate potential issues and benefit a client in the litigation process. Building a relationship between a lawyer and a client that both manages and monitors social media use can further aid a client’s case or deter any issues that may arise. Remember, social media posts may not accurately represent a person’s everyday life, which can ultimately affect what a client deserves to receive as compensation for their loss.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
After the Event Insurance: The New Legal Safety Net
Personal Injury Client Costs and Fees
In Ontario automobile and non-automobile personal injury cases, the costs and fees can be a heavy burden for a client. Generally, lawyers and clients establish a Contingent Fee Agreement (CFA) where a client agrees to pay the lawyer’s costs only if successful. If the case is unsuccessful, a client does not have to pay the lawyer’s costs. However, the client may still have to pay the lawyer’s outstanding disbursements.
Adverse Cost Award
The adverse cost award rule requires that an unsuccessful party pay a portion of the winning party’s disbursements. However, even if a client is successful they may still have to pay a portion of the opposing party’s costs and fees if the opposing party made an offer to settle before trial and the award is less favourable than the settlement offer.
Please see below for detailed explanations of costs and disbursements, the adverse cost award, and settlement offers rule.
What Is After the Event (ATE) Insurance?
 After the Event (ATE) insurance is a legal expense Insurance policy now available in Ontario that covers some of the fees and disbursements at the end of a case or settlement. ATE Insurance is one of the most effective ways to protect a client financially after the trial process and provide a safety blanket if unsuccessful. Before deciding to purchase ATE insurance it is important to understand how ATE Insurance works and its implications in the trial process. ATE Insurance benefits can vary widely depending on the policy you purchase, settlement offers, and the outcome of your case.
After the Event (ATE) insurance is a legal expense Insurance policy now available in Ontario that covers some of the fees and disbursements at the end of a case or settlement. ATE Insurance is one of the most effective ways to protect a client financially after the trial process and provide a safety blanket if unsuccessful. Before deciding to purchase ATE insurance it is important to understand how ATE Insurance works and its implications in the trial process. ATE Insurance benefits can vary widely depending on the policy you purchase, settlement offers, and the outcome of your case.
Common Questions about ATE Insurance
1) What’s in it for the Firm?
We don’t make a profit.
Our only incentive to provide the ATE Insurance option is to protect our clients and provide a safety net if needed.
By providing the ATE Insurance product through a specified broker we are also able to offer a lower premium rate because the product is purchased as a group rate which is offered to all of our eligible clients.
2) What are costs and disbursements?
Costs are defined as a portion of legal fees of one party that the opposing party must pay usually if they are unsuccessful.
Disbursements are other legal expenses such as court fees, travel costs, experts, printing, office expenses, and more.
Generally, an unsuccessful party must pay 60% the costs and disbursements of the opposing party. However, a judge has discretion to compel a party to pay up to 100% of the costs and disbursements depending on each case.
3) Who is our ATE Insurance brokerage?
The Judge is an Insurance brokerage working in the litigation field. The Judge focuses on providing clients with financial protection by covering unsuccessful litigation costs. The goal of The Judge is to encourage affordable access justice.
4) Who is the policy holder?
The plaintiff is usually always the policy holder.
5) How much does ATE Insurance premium cost?
The standard premium rate is $1,350 (not including taxes), which covers $100,000 in costs and disbursements. These rates can vary widely between $25,000 and $250,000. The premiums can reach between $2,500 and $3,500 depending on projected costs of litigation.
Policy terms can vary from each case and insurer.
6) When do you have to pay?
Premiums are deferred until a case concludes.
The premium is only paid if the plaintiff is successful and does not face any adverse cost awards.
7) How does the ATE Insurance premium work?
If you are awarded under $10,000 there is no premium owed. If you lose and the court awards costs against you, the insurance company will cover those costs up to $100,000 and no premium will be charged as well.
8) When can ATE Insurance be purchased?
ATE Insurance is acquired ideally within six months of retaining a law firm. However, it can be purchased later at an increased premium.
9) What does the ATE Insurance policy cover?
A typical policy will be triggered by one of these events:
- You are unsuccessful at trial and are required to pay defence costs and disbursements awarded at trial.
- You are successful but failed to beat a settlement offer by the opposing party.
- If you seek to abandon a claim, disbursements may be covered.
10) What is an offer to settle?
Generally, any party in litigation can make an offer to settle at any time. To ensure that it is recognized by the court as a valid offer to settle it should be made at least seven days before a hearing.
11) How do offers to settle affect costs and disbursements?
There are litigation rules that affect the outcome of costs and disbursements in a case where a settlement offer was rejected. Where an offer to settle is made and the opposing party rejects the offer, the costs and disbursements may be changed depending on the outcome of the trial.
Example: Where the opposing party makes an offer to settle, the offer is not withdrawn, and the plaintiff rejects the offer.
- If you are successful at trial but receive a judgment as favourable or less favourable than the settlement offer the plaintiff rejected, you will generally have to pay 60% of the opposing party’s costs and disbursements from the date the settlement was offered onward. The judge has discretion to compel the claimant to pay a higher percentage of costs and disbursements depending on each case.
- If you are unsuccessful at trial and the opposing party receives a judgment as favourable or less favourable to the settlement offer the plaintiff rejected, the opposing party is entitled to 90% of the costs and disbursements of the plaintiff from the date the offer to settle was made.
It is important to remember that because of the “offer to settle” rule, the plaintiff may be faced with adverse costs despite being successful in a case.
12) How many cases settle?
Approximately 96% of cases settle annually.
13) What does ATE Insurance not cover?
ATE Insurance does not cover the plaintiff’s lawyer legal fees.
Minimize the Financial Risk and Uncertainty of Litigation with ATE Insurance
For our clients, the primary advantage of purchasing ATE insurance is the peace of mind it provides knowing that, regardless of the outcome, potential costs will be covered.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
Members of Our Legal Team Completed the Ontario Brain Injury Association’s Brain Basics Training Program
The Ontario Brain Injury Association’s (OBIA’s) Brain Basics Training Program is a foundational course that gives professionals, caregivers, and survivors alike the opportunity to develop a holistic understanding of how the brain works.
We are always seeking ways to improve ourselves individually and as a group. Towards this end, we are proud to announce that Stephanie, Harpreet, and Rusald, members of our legal team, recently completed the Brain Basics Training Program.
Click here to learn more about our team.
Despite the name, mild traumatic brain injuries (mTBIs) are serious and complex injuries. To truly understand how brain injuries manifest and are treated an understanding of the brain itself—how it’s structured and operates—is essential. The OBIA’s Brain Basics course equips our legal team with knowledge that enables us to better help and serve our clients.
Roger R. Foisy is an experienced Personal Injury Lawyer in Ontario who has helped clients with brain injuries receive compensation. If you or a loved one has suffered a brain injury, please contact us for immediate support and a free consultation.
*Roger R. Foisy has completed courses in Neurorehabilitation, Neurobehavioral Disorders, Advanced Brain Injury Rehabilitation, Cognitive Interventions for Adults with Acquired Brain Injuries, and Neuropsychological Assessments: Beyond Testing from Brock University. However, he is not a medical professional. The advice in this blog is not intended as a substitute for medical advice.
More on Brain Injury from Roger R. Foisy:
How Mild Traumatic Brain Injuries (mTBIs) Affect the Family
Suffering an mTBI can be a life altering event for a person, disrupting their day-to-day routines and leaving them feeling scared, vulnerable, and confused. It is important to remember, however, that the effects go beyond the individual—changing the lives of close family members who in many cases are the first line of support.
In this article, I look at how an mTBI diagnosis impacts the family, paying particular attention to those closest to the injured individual who play an instrumental role in the recovery process.
Understanding the Impact of an mTBI on the Individual
A traumatic brain injury is any physical injury to the brain that causes a disruption of normal functioning. Although 70-90% of all traumatic brain injuries are classified as mild, that does not mean they are not serious. The reality is that any injury that upsets your brain’s normal functioning, even if it is only temporary, needs to be taken very seriously.
mTBIs do not discriminate based on factors like a person’s age, sex, or overall health. They can impact anyone, whether a slip and fall resulting in a head injury or an adult who suffers a whiplash injury during a motor vehicle accident.
Symptoms of an mTBI are commonly broken down into three categories—physical, cognitive, and emotional—and include:
- Physical: Headaches, ringing in the ear, dizziness, insomnia, fatigue, and the loss of one or more of the five senses.
- Cognitive: Attention, concentration, memory, information processing, reasoning, and planning.
- Emotional: Irritability, depression, anxiety, and mood swings.
Remember that, because each individual and injury is unique, no two mTBIs will be alike. One person might display more physical symptoms, another more emotional, and another more cognitive. Sometimes symptoms present suddenly, while in other cases they may not appear for weeks afterwards. Understanding the effects an mTBI has on the specific person will lead to better treatment and support.
The Role of the Family in Supporting the Individual
Watching a loved one suffer with an mTBI and supporting them as they recover can be a difficult experience for a family. When one person in a household experiences an mTBI, everyone feels it.
 It is not uncommon for those close to the affected individual to struggle with emotions like denial, sadness, anger, frustration, and guilt. You need to be patient with yourself and understand that these feelings are normal responses to what can be significant life changes. To learn more about common emotional responses and how to cope with them, I invite you to read my earlier article on this subject.
It is not uncommon for those close to the affected individual to struggle with emotions like denial, sadness, anger, frustration, and guilt. You need to be patient with yourself and understand that these feelings are normal responses to what can be significant life changes. To learn more about common emotional responses and how to cope with them, I invite you to read my earlier article on this subject.
In the days and weeks that follow an mTBI event and diagnosis, family members often find themselves providing two types of support:
- Attendant Care: This kind of assistance is often more supervisory in nature and includes duties such as making sure individuals do not leave appliances like stoves and ovens turned on and that they take their medications as required. Depending on how their symptoms manifest, some individuals might require physical help to stand up or walk between rooms, though these needs tend to prevail earlier on, usually due to dizziness, and be short lived.
- Caregiving and Emotional Support: This is the emotional piece and can be more drawn out as those impacted grapple with the long-term effects of an mTBI. At this stage, individuals suffering from an mTBI might be more prone to lashing out at those closest to them and acting irritably as a response to feelings of anger, frustration, and depression. Being there for the individual reminds them that together you will get through this challenging period.
 One of the most important things to emphasize is that family members looking after a loved one with an mTBI also need to make sure they are looking after themselves. This is a problem I have seen firsthand especially in situations where the symptoms are more severe and long lasting. Parents, for example, can become so invested in their children getting better that they do not see the effect their son or daughter’s injury is having on them.
One of the most important things to emphasize is that family members looking after a loved one with an mTBI also need to make sure they are looking after themselves. This is a problem I have seen firsthand especially in situations where the symptoms are more severe and long lasting. Parents, for example, can become so invested in their children getting better that they do not see the effect their son or daughter’s injury is having on them.
As much as you would like to be there, you simply cannot be present 24/7. Watch out for each other as a family and, if you feel one member is pushing themselves too much, encourage them to take a personal respite so they can rest and recharge.
Aiding Your Family in the Aftermath of an mTBI Diagnosis
The Ontario Brain Injury Association (OBIA) is a good resource for individuals and their loved ones suffering from an mTBI. In addition to providing information for people in Ontario who are living with brain injuries, the OBIA also has a helpline (1-800-263-5404) to provide caring and compassionate support.
Roger R. Foisy is an experienced Personal Injury Lawyer in Ontario who has helped clients with brain injuries receive compensation. If you or a loved one has suffered a brain injury, please contact us for immediate support and a free consultation.
*Roger R. Foisy has completed courses in Neurorehabilitation, Neurobehavioral Disorders, Advanced Brain Injury Rehabilitation, Cognitive Interventions for Adults with Acquired Brain Injuries, and Neuropsychological Assessments: Beyond Testing from Brock University. However, he is not a medical professional. The advice in this blog is not intended as a substitute for medical advice.
More on Brain Injury from Roger R. Foisy:
Recognizing the Signs and Symptoms of a Concussion [Infographic]
June is Brain Injury Awareness Month. Every year approximately 160,000 Canadians sustain brain injuries, the majority of which are concussions.
Unfortunately, because people often think of a concussion as “just a concussion”, trauma to the brain can easily be overlooked. It is important that a concussion always be taken seriously. Regardless of how mild it might appear to be, it is still a traumatic brain injury and can have far-reaching impacts on a person’s life.
After suffering a concussion, a person will often experience symptoms that are:
- Emotional
- Physical
- Cognitive
Remember that, because each injury is unique, symptoms and effects will manifest differently between individuals. Being aware of the emotional, physical, and cognitive symptoms to watch for will make it easier to seek help and treatment in a timely manner and facilitate a better recovery.
No Title
No Description
Roger R. Foisy is an experienced Personal Injury Lawyer in Ontario who has helped clients with brain injuries receive compensation. If you or a loved one has suffered a brain injury, please contact us for immediate support and a free consultation.
*Roger R. Foisy has completed courses in Neurorehabilitation, Neurobehavioral Disorders, Advanced Brain Injury Rehabilitation, Cognitive Interventions for Adults with Acquired Brain Injuries, and Neuropsychological Assessments: Beyond Testing from Brock University. However, he is not a medical professional. The advice in this blog is not intended as a substitute for medical advice.
I Encourage You to Watch My Mild Traumatic Brain Injury Video Series:
- What is a Mild Traumatic Brain Injury (mTBI)?
- Why Are Mild Traumatic Brain Injuries Often Missed?
- Accessing Funding for Medical Rehabilitation after Suffering a Mild Traumatic Brain Injury in a Motor Vehicle Accident
- Finding the Right Team for Your Mild Traumatic Brain Injury
- Coping with the Emotional and Psychological Impact of a Mild Traumatic Brain Injury
Dress Down for Brain Injury Awareness Month This June
This coming June is Brain Injury Awareness Month. In Canada, approximately 160,000 Canadians suffer brain injuries every year with incidence and reporting rates continuing to rise. The prevalence of brain injury outpaces breast cancer, multiple sclerosis, spinal cord injury, and HIV/AIDS combined, and it remains the number one killer and disabler of people under 44.
To raise awareness and funds in support of Brain Injury Awareness Month, my team and I will be launching an event—Dress Down for Brain Injury Awareness Month. Every Friday, each of us will contribute $5 so we can enjoy wearing casual clothes for the day. At the end of the month, the firm will match those donations 100% and give all proceeds to the Ontario Brain Injury Association.
I encourage you to join us by having your own office take part in Dress Down for Brain Injury Awareness Month, matching whatever amount you are comfortable with to help us support this important and worthwhile cause.
Roger R. Foisy is an experienced Personal Injury Lawyer in Ontario who has helped clients with brain injuries receive compensation. If you or a loved one has suffered a brain injury, please contact us for immediate support and a free consultation.
*Roger R. Foisy has completed courses in Neurorehabilitation, Neurobehavioral Disorders, Advanced Brain Injury Rehabilitation, Cognitive Interventions for Adults with Acquired Brain Injuries, and Neuropsychological Assessments: Beyond Testing from Brock University. However, he is not a medical professional. The advice in this blog is not intended as a substitute for medical advice.
More on Brain Injury from Roger R. Foisy:
- Personal Injury Potential Settlement Values: Mild Traumatic Brain Injury
- New Concussion Blood Test Developed with a 90% Accuracy Rate!
- How Speech-Language Pathologists Help Traumatic Brain Injury Victims
Understanding Why OHIP Might Receive Part of Your Injury Claim Settlement
After receiving a personal injury claim settlement, you might discover that you are not the only beneficiary. Many clients are surprised to learn that a third party – such as the Ontario Health Insurance Plan (OHIP) – might also be entitled to payment of its own claim.
This is known as “subrogated interest”.
It is important for injury victims to understand what subrogated interest is and how it can relate to their case. In this article, I will answer some common questions about subrogated interest and discuss why, when, and how OHIP claims it:
What Is Subrogated Interest?
Subrogation is a legal right afforded to insurance companies to recover the amount they have paid for a loss by suing the party that caused the loss.
In certain situations, OHIP will cover healthcare costs associated with things like physician and hospital services, diagnostic testing and imaging, and more. If these are necessary as a result of someone else’s wrongdoing, OHIP is entitled to pursue compensation.
 In their article on this topic, the Ontario Trial Lawyers Association (OTLA) presented this example: Imagine Mr. A was the victim of a blundered surgery. He would need to seek subsequent medical services, which OHIP would provide, and then sue the doctor who performed the initial operation (Dr. B) for the damage. Since Dr. B was responsible, OHIP can make a claim and expect to be reimbursed for the expenses associated with Mr. A’s care.
In their article on this topic, the Ontario Trial Lawyers Association (OTLA) presented this example: Imagine Mr. A was the victim of a blundered surgery. He would need to seek subsequent medical services, which OHIP would provide, and then sue the doctor who performed the initial operation (Dr. B) for the damage. Since Dr. B was responsible, OHIP can make a claim and expect to be reimbursed for the expenses associated with Mr. A’s care.
In the majority of cases, OHIP will essentially “piggyback” on a claimant’s lawsuit. Neither OHIP nor the claimant will recover anything if the case is not successful, however OHIP can pursue financial reimbursement if you reach a settlement.
What Costs Can and Can’t OHIP Recover through Subjugated Interest?
OHIP can recover healthcare and treatment costs stemming from a range of things like slips and falls, medical malpractice or professional negligence, class action, product liability or manufacturing defects, and boat, air, or rail accidents.
Services for which OHIP can be reimbursed include:
- Physician treatments
- Hospital visits and stays (in/out patient, acute, and chronic care)
- Out-of-province or out-of-country medical services
- Extended care
- Professional services like nursing, occupational therapy, physiotherapy, speech-language therapy, and others
- Personal and attendant care services
- Long-term care accommodation
- Community support
In addition to being compensated for services already provided, OHIP can seek reimbursement for the costs of future OHIP-insured services such as those administered by a physician or hospital. What OHIP can’t claim for are future non-professional healthcare or benefit services like personal support or homecare. Your lawyer should factor these expenditures into your personal claim for damages so you can purchase these services directly once you receive the funds.
Can OHIP Recover Costs Associated with Automobile Accidents?
 OHIP cannot make subrogated interest claims related to motor vehicle accidents. It is limited by the Insurance Act and Health Insurance Act, the latter stating that:
OHIP cannot make subrogated interest claims related to motor vehicle accidents. It is limited by the Insurance Act and Health Insurance Act, the latter stating that:
“…the Plan is not subrogated to the rights of the insured person, as against a person who is insured under a motor vehicle liability policy issued in Ontario, in respect of personal injuries arising directly or indirectly from the use or operation…”
In other words, OHIP can’t advance a subrogated interest claim against someone insured under an Ontario motor vehicle liability policy for injuries arising from the operation of an automobile. This is because insurers already pay an annual levy of around $150 million to OHIP to specifically address car accident-related injuries. Based on the number of recent changes to the medical and rehabilitation benefits limit afforded to accident victims under the no-fault accident benefits portion of their automobile policy, it is very likely that this levy is not nearly enough to cover the expected health care services OHIP can expect to cover from car accident victims when their benefits run out!
Can Other Parties Besides OHIP Make Subrogated Interest Claims?
In addition to OHIP, other groups that might be able to claim subrogated interest include:
- The Workplace Safety and Insurance Board (WSIB)
- The Criminal Injury Compensation Board (CICB)
- Group Insurance Policies
Applicability varies on a case-by-case basis, and there are important limitations.
For example, while OHIP can recover costs through subrogation with “quasi motor vehicle cases” (those where there are both motor vehicle and non-motor vehicle defendants), the Insurance Act expressly prohibits Group Insurance Policies from ever doing so.
Taking Subrogated Interest into Account in Your Claim
When a third party like OHIP covers costs associated with treatment and care after an injury, it makes sense for them to seek compensation when you receive funding for your recovery.
Your lawyer should work with you to understand if subrogated interest is applicable in your case and, if it is, ensure you are prepared by taking all relevant costs into account. This will enable you to reimburse all relevant third parties and cover your own ongoing expenses after you are awarded your settlement.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
- 3 Reasons the Pain and Suffering Cap Should Be Abolished
- Personal Injury Potential Settlement Values: Scarring and Disfigurement of the Face and Neck
- How Speech-Language Pathologists Help Traumatic Brain Injury Victims
How to Avoid Being Denied Disability Benefits: Completing the Physician Statement [Video]
As an Ontario Long Term Disability lawyer, I am regularly asked how people can avoid being denied LTD benefits when they are applying.
From a legal action perspective, I can only accept long term disability clients after their application has been denied or their benefits have been wrongfully terminated. However, I am able to give some helpful guidelines based on my years of experience seeing common errors that lead to LTD application denials.
In this video, I focus on your physician’s statement for the LTD application, and the critical role they play in whether your application is approved or denied. I offer advice on how to work with your medical practitioner(s) to ensure your application has a better chance of being approved.
Although your physician has your best interests at heart, insurance adjusters regularly deny LTD claims because the physician has not provided enough information to understand why you can’t return to work. It’s critical for your physician’s statement to include the connection between your injury or illness and why those symptoms prevent you from being able to complete the primary duties of your employment.
Watch my video below for the LTD Physician Statement walkthrough:
If you found this video helpful, I encourage you to watch my other videos in this series, which provide guidance about the section you must complete as well as the section completed by your employer. Each of these sections are critical to the success of your LTD application.
Unfortunately, many people face denied claims and termination of long term disability benefits every day. Knowing how to fill out the application forms will increase your chances of being approved, so you can receive the benefits you need for your recovery process.
If you have applied for LTD benefits and have been wrongfully denied, or if your LTD benefits have been recently terminated, contact us for immediate support and a free consultation.
See all of my Long Term Disability videos for answers to common questions.
More long term disability information from Roger R Foisy:
- The Long Term Disability Insurance Process and Why It Can Fail
- Do You Understand the Definition of Disability in Your Group Insurance Policy?
- Why Insurance Companies May Have You Under Surveillance (And How You Can Lose Your Long Term Disability Compensation)
How to Avoid Being Denied Disability Benefits: Completing the Sponsor (Employer) Statement [Video]
As an Ontario Long Term Disability lawyer, I am regularly asked how people can avoid being denied LTD benefits when they are applying.
From a legal action perspective, I can only accept long term disability clients after their application has been denied or their benefits have been wrongfully terminated. However, I am able to give some helpful guidelines based on my years of experience seeing common errors that lead to LTD application denials.
In this video, I discuss how to work with your employer so they can properly complete their section of the LTD application, often referred to as the Plan Sponsor Statement. These tips will help your application be less likely to be denied.
Your employer’s submission about your job will be considered more heavily than yours. For this reason, it’s essential that both you and your employer give consistent accounts of what your primary job duties are, and how your injury or illness affects your ability to carry out those duties.
Watch my video below for the LTD Plan Sponsor (Employer) Statement walkthrough:
If you found this video helpful, I encourage you to watch my other videos in this series, which provide guidance about the section you must complete as well as the section completed by your treating physician. Each of these sections are critical to the success of your LTD application.
Unfortunately, many people face denied claims and termination of long term disability benefits every day. Knowing how to fill out the application forms will increase your chances of being approved, so you can receive the benefits you need for your recovery process.
If you have applied for LTD benefits and have been wrongfully denied, or if your LTD benefits have been recently terminated, contact us for immediate support and a free consultation.
See all of my Long Term Disability videos for answers to common questions.
More long term disability information from Roger R Foisy:
How to Avoid Being Denied Disability Benefits: Completing the Member Statement [Video]
 As an Ontario Long Term Disability lawyer, I am regularly asked how people can avoid being denied LTD benefits when they are applying.
As an Ontario Long Term Disability lawyer, I am regularly asked how people can avoid being denied LTD benefits when they are applying.
From a legal action perspective, I can only accept long term disability clients after their application has been denied or their benefits have been wrongfully terminated. However, I am able to give some helpful guidelines based on my years of experience seeing common errors that lead to LTD application denials.
In this video, I walk you through the important and problematic components of the section you are required to complete in the LTD application process, often referred to as the Plan Member Statement. I provide tips to give your application a better chance of success.
For example, I discuss how it’s essential to elaborate on each issue that affects your ability to work. Although the form may not give you ample room for comments, you can include a note such as “see attached” in the comment field, and include a separate paper with additional information with your application.
Watch my video below for the LTD Plan Member Statement walkthrough:
If you found this video helpful, I encourage you to watch my other videos in this series, which provide guidance about the sections completed by your employer and your treating physician. Each of these sections are critical to the success of your LTD application.
Unfortunately, many people face denied claims and termination of long term disability benefits every day. Knowing how to fill out the application forms will increase your chances of being approved, so you can receive the benefits you need for your recovery process.
If you have applied for LTD benefits and have been wrongfully denied, or if your LTD benefits have been recently terminated, contact us for immediate support and a free consultation.
See all of my Long Term Disability videos for answers to common questions.
More long term disability information from Roger R Foisy:
3 Reasons the Pain and Suffering Cap Should Be Abolished
What Is Pain and Suffering in Terms of Personal Injury Law?
Pain and suffering is a type of damage that an injured party may claim during a lawsuit. It is considered a “non-pecuniary” damage, which is a loss that is not easily quantifiable in financial terms (as opposed to, for example, loss of wages).
Compensation for pain and suffering is intended to cover for the loss of enjoyment, the impact the injury has on the victim’s daily life, and the stress caused by the injury (both physical and emotional/psychological). As such, pain and suffering claims depend on each individual’s circumstances. Certain types of injuries will have a long-lasting effect on the rest of your life – no monetary value can truly compensate for this.
Due to the challenge of putting a value on this type of loss, judges will base the award on damages awarded in previous similar cases with guidance from appeal courts like the Supreme Court of Canada.
What Is the Pain and Suffering Cap?
The Supreme Court of Canada set an upper limit, or “cap”, on pain and suffering damages in 1978, based on the case Andrews v. Grand & Toy Alberta Ltd. in which the 21-year-old Andrews was rendered quadriplegic in a motor vehicle accident.
Pain and suffering was capped at the amount Andrews received for this portion of the claim: $100,000 (which is approximately $369,000 in today’s dollars).
For personal injury victims who come before the court today, this amount often seems inconsequential in the face of the injuries they have suffered and the pain and loss they will struggle with for the rest of their lives. Many personal injury lawyers, such as myself, believe that this cap does not serve the best interests of the victims and instead does them an injustice.
Motor Vehicle Accidents: Pain and Suffering Threshold and Deductible
On top of the pain and suffering cap, motor vehicle accident (MVA) victims must contend with a “threshold” and a deductible.
- Threshold:
If you’re injured in an MVA, in order to include pain and suffering in your case, you must first show that you sustained permanent serious impairment of an important physical, mental, or psychological function, or permanent serious disfigurement such as scarring.
- Deductible:
If your case meets the threshold, you may be entitled to recover pain and suffering damages. However, in Ontario awards for pain and suffering in MVA cases are automatically reduced by a current deductible of $37,385.17 unless your pain and suffering award exceeds $124,616.21. Jurors are not informed about this deductible when making their Judgments.
The threshold and deductible requirements for MVAs are increasing year-over-year, further limiting a victim’s ability to receive compensation. These rules act in favour of the insurer or defendant. This is not surprising, given the extensive recent history of auto insurance coverage being slashed and restrictions placed MVA personal injury law cases.
Motor vehicle accident victims – and all personal injury victims – deserve better from the justice system.
3 Reasons to Abolish the Pain and Suffering Cap
The Ontario Trial Lawyers Association (OTLA) has published an article giving three excellent reasons to abolish the pain and suffering cap, which I will echo here:
- Other general damages, such as defamation, do not have a cap. This means victims can be awarded more for something like the loss of reputation than they can for loss of limb.
- As mentioned above, MVA victims face additional insurance deductibles. This creates an unfortunate situation where victims are stricken with both a damages cap and a large insurance deductible.
- Pain and suffering damages can be calculated in a more objective and quantifiable way. For example, in the United States juries are asked to consider the hourly value of the pain and suffering and calculate it over a lifetime, or use a multiple of the economic damages since losses to health, independence, and quality of life pale in comparison to economic losses.
Click here to read the full article from OTLA.
Recent Progress in Ending the Pain and Suffering Cap
Although the cap has not been abolished, we have recently seen a promising development that suggests the time of the pain and suffering cap may be coming to an end.
A recent case on April 20, 2017 McKnight v. Her Majesty the Queen et al., in Brantford, Ontario, included a $600,000 award for pain and suffering damages.
This is a step in the right direction, and a sign that the courts are recognizing that the pain and suffering cap is unjust to victims. While no amount of money can truly compensate injury victims for their pain and suffering over a lifetime, abolishing the pain and suffering cap would at least help to ease their financial burden.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
- Quantifying Damages: Housekeeping and Home Maintenance
- Quantifying Damages: Personal and Attendant Care
- New Resource! Personal Injury Potential Settlement Values
Merry Christmas and Happy New Year from the Roger R Foisy Law Firm!
A very Merry Christmas to you and your loved ones from the Roger R Foisy team! We hope you have a wonderful holiday filled with joy and relaxation, and we wish you health and happiness in 2018.
Our Holiday Hours
- December 15: Closed from 9:30 am – 2:30 pm for Knights Table charity volunteering event.
- December 22: Closed at 2:30 pm.
- December 25 – 26: Closed.
- December 27 – 29: Open.
- January 1: Closed.
Our 12 Days of Christmas
At the Roger R Foisy Law Firm, we have been leading up to Christmas with festivities at the office (cookies and potlucks and gingerbread houses, oh my!) along with charitable donations.
Here are a few of the charities we are contributing to over the holidays – we encourage you to spread some holiday cheer to these organizations if you are able this season:
- Eden Food for Change: An organization that provides access to food for families in Western Mississauga who are in need.
- Knights Table: An organization that serves the needs of people dealing with issues of poverty and homelessness in the Peel Region.
- CP24 CHUM Christmas Wish: One of the largest distributors of toys to children in need in the Greater Toronto Area, as well as a provider of financial assistance to hundreds of agencies.

Season’s Greetings from Roger R Foisy to you and your family. Stay safe this Christmas season!
Learn about personal injury from Roger R Foisy:
Personal Injury Potential Settlement Values: Scarring and Disfigurement of the Face and Neck
Catastrophic injuries can cause scarring and disfigurement that can have a lifelong impact, physically, psychologically, and emotionally. The high visibility of scarring and disfigurement on the side of the face and neck can also affect a person’s quality of life in numerous ways, such as lost employment opportunities and low self-esteem.
It is important for the injured person to understand that their psychological and emotional reactions are valid and normal. In most cases, victims are compensated for the psychological injury as well as the physical injury.
In this article, we will take a look at a historical example of the personal injury settlement values victims have received:
Potential Settlement: Scarring and Disfigurement on the Face and/or Neck
In 2012, the Court in Ellis v Fallios-Guthierrez, 2012 ONSC 1670 awarded the injured person $55,000 for injuries that included scarring and disfigurement of the face.
To read the full decision, click here.

Receiving the Settlement You Deserve
People often believe that settlement value is mostly determined by the extent of the injury. While this is a factor, the most important information is how the injury has impacted your life. In other words, what does the injury prevent you from being able to do and how does this affect you?
I encourage you to view my previous article about seeking compensation for the psychological impact of scar, burn, or disfigurement injuries, wherein I discuss, in greater detail, how victims can receive the compensation they deserve.
A thorough lawyer should take the time to fully understand your specific situation, including your life and responsibilities before and after your accident, to ensure you do not under-settle your case. By quantifying every possible loss, you are more likely to receive a just settlement that will help to ease the financial burdens that usually occur during recovery.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
Personal Injury Potential Settlement Values: Basal Skull Fracture
A basal skull fracture, most often caused by motor vehicle accidents, slip and fall accidents, and child abuse cases, is considered a severe head injury. It is a fracture at the base of the skull and is frequently accompanied by a brain injury, which can cause significant challenges for victims.
Some symptoms include:
- Racoon (black) eyes
- Loss of sensation to forehead
- Loss of sensation to lower face
- Ringing in the ears (tinnitus)
- Deafness
- Bleeding from nose and/or ears
A basal skull fracture is not usually confirmed without the use of an x-ray or CT scan.
In this article, we will take a look at a historical example of the personal injury settlement values victims have received for this injury:
Potential Settlement: Basal Skull Fracture
In 2003, the Court in White v Aransibia, [2003] OJ No 2580 awarded the injured person $100,000 for injuries that included a basal skull fracture.
To read the full decision, click here.
Receiving the Settlement You Deserve
People often believe that settlement value is mostly determined by the extent of the injury. While this is a factor, the most important information is how the injury has impacted your life. In other words, what does the injury prevent you from being able to do and how does this affect you?
I encourage you to view my previous article about seeking compensation for a basal skull fracture, wherein I discuss, in greater detail, the injury and how victims can receive the compensation they deserve.
A thorough lawyer should take the time to fully understand your specific situation, including your life and responsibilities before and after your accident, to ensure you do not under-settle your case. By quantifying every possible loss, you are more likely to receive a just settlement that will help to ease the financial burdens that usually occur during recovery.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
Are You Ready for Back to School? (ICE Program and Auto Insurance Coverage)
 As September comes into full swing, the kids are now back to school. While it’s an exciting time for families, it can lead to worries about safety.
As September comes into full swing, the kids are now back to school. While it’s an exciting time for families, it can lead to worries about safety.
Unfortunately, accidents can happen whether a child walks to school on their own or their parent drives them in. The best way to face the possibility of an accident is to be prepared – preparation can make a real difference in an emergency situation.
Below, I discuss a few ways families can prepare now for unexpected accidents:
ICE Program
The “In Case of Emergency” (ICE) program is recognized internationally by first responders and emergency services personnel. An ICE card has the name and phone number of two emergency contacts, which the first responders can use to quickly reach the injured person’s immediate family.
Children going back to school can carry an ICE card with them, on their jacket, backpack, or in their bicycle helmet, giving parents peace of mind that they would be immediately contacted if anything were to happen.
We offer this program free of charge. Click here to find out more and get your ICE card.
Auto Insurance Coverage
Auto insurance has suffered massive cuts to coverage in recent years, and has become even more difficult to qualify for. These reduced benefits are highly unlikely to be sufficient to cover medical, rehabilitation, and attendant care costs if you or your child are seriously injured in a motor vehicle accident.
Parents can take steps to protect themselves and their families. I highly recommend purchasing additional coverage in your auto insurance policy – it’s very affordable and can make a substantial difference.
I’ve put together this infographic to showcase this issue. I encourage you to share it with other Ontario drivers and parents:
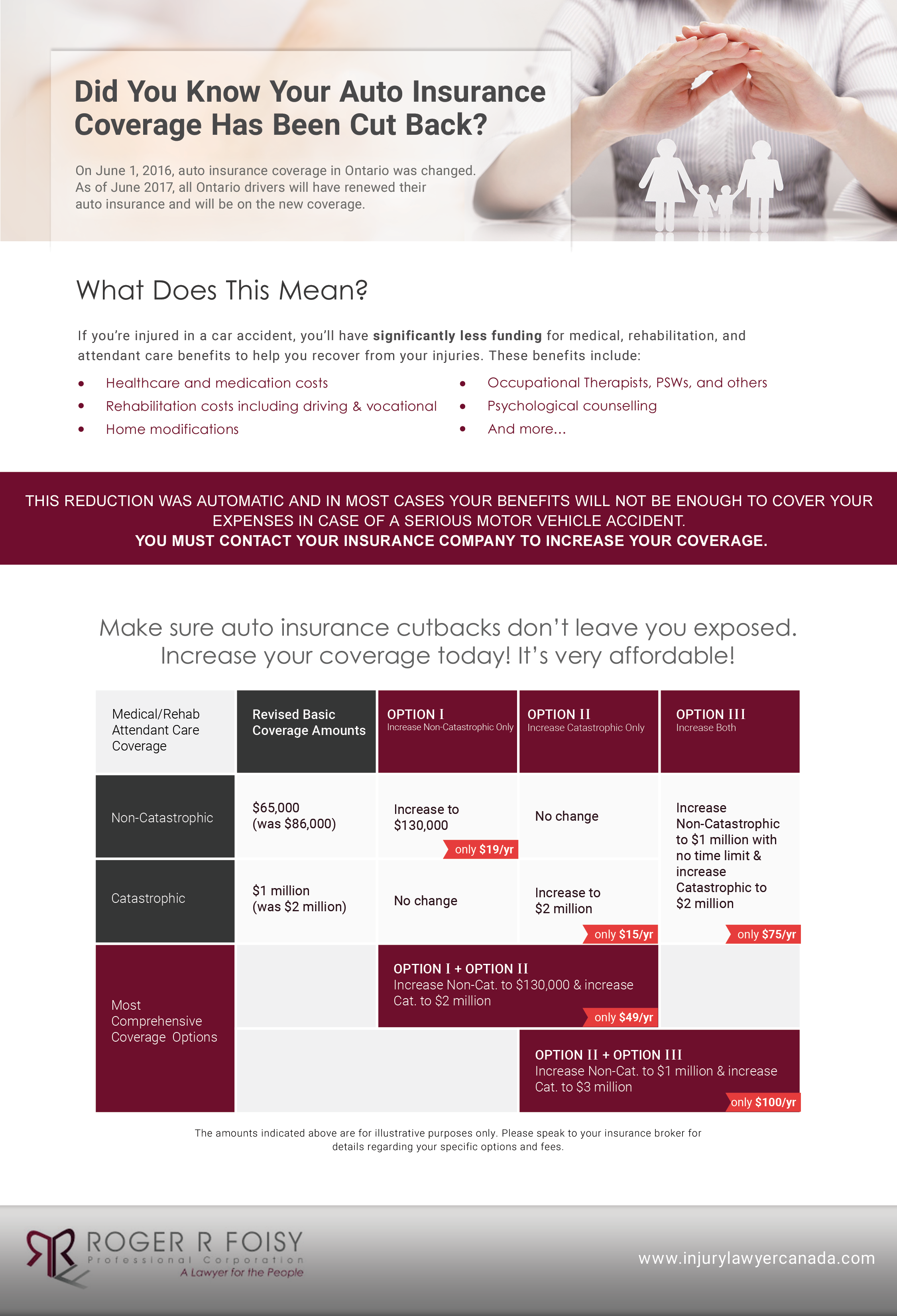
From all of us at the Roger R. Foisy law firm, stay safe during back to school season this year!
More from Roger R. Foisy:
Roger R. Foisy Completes Executive Certificate in Conflict Management
 I am always working to improve myself as a lawyer, so I can better help my clients and achieve the best possible outcomes for them. As of July 21, 2017, I have completed an Executive Certificate in Conflict Management through the Stitt Feld Handy Group in association with the University of Windsor Law School.
I am always working to improve myself as a lawyer, so I can better help my clients and achieve the best possible outcomes for them. As of July 21, 2017, I have completed an Executive Certificate in Conflict Management through the Stitt Feld Handy Group in association with the University of Windsor Law School.
The certificate involved in-class training and workshops focused on advanced negotiation skills, dispute resolution skills, dealing with difficult people, and successfully navigating difficult situations. Through a combination of lectures, demonstrations, videos, and coached case studies, as well as group discussions and exercises, participants emerge with immediately applicable, practical skills. Read more about this certificate here.
Successful conflict resolution is a critical skillset for any personal injury and long-term disability lawyer, particularly during litigation and when securing a fair settlement. As you may expect, my client’s position will often be strongly opposed to the insurance company’s position; and my role is to successfully mediate and guide the interaction between these conflicting viewpoints to ensure my client receives a beneficial settlement.
Likewise, my clients themselves have often gone through a traumatic experience and may be suffering from chronic pain. They are anxious, uncertain, and stressed about the outcome of the settlement. My role also includes understanding my clients and helping them as they cope with the difficult situations they are faced with.
As I have detailed previously, I frequently attend workshops, seminars, and courses in order to become more knowledgeable and update my skills. I believe this is an essential duty for any personal injury lawyer, as it allows them to provide their clients with the best possible support.
Roger R. Foisy is an Ontario Personal Injury Lawyer with extensive experience in personal injury, long-term disability, and brain injury. Please contact us for immediate support and a free consultation.
Click here to watch my video series about personal injury law.
More from Roger R. Foisy:
Personal Injury Potential Settlement Values: Whiplash Injuries
Whiplash injuries are generally the result of the head snapping forward and then back again, especially in rear-end motor vehicle accidents. Other similar activities gone wrong can cause a whiplash, such as a roller coaster, skiing, or from a sports injury where you might be accidently hit, kicked, or shaken.
This rapid movement can strain, stretch, or tear muscles and tendons in the neck, causing injury. It can also cause mild to moderate traumatic brain injuries.
The below video is a brief animation of what happens inside the head when a whiplash motion occurs:

In this article, we will take a look at the four classifications of whiplash injuries and historical examples of the personal injury settlement values victims have received:
Potential Settlement: Whiplash Associated Disorder I
WAD I commonly results in stiffness or tenderness in the neck.
In 2012, the Court in Clark v. Kouba, 2012 BCSC 1607 awarded the injured person $85,000 for injuries that included WAD I.
To read the full decision, click here.

Potential Settlement: Whiplash Associated Disorder II
WAD II commonly results in a decreased range of motion and tenderness in the neck.
In 2009, the Court in Watts v. Donovan, 2009 CanLII 26931 (ON SC) awarded the injured person $95,000 for injures that included WAD II.
To read the full decision, click here.
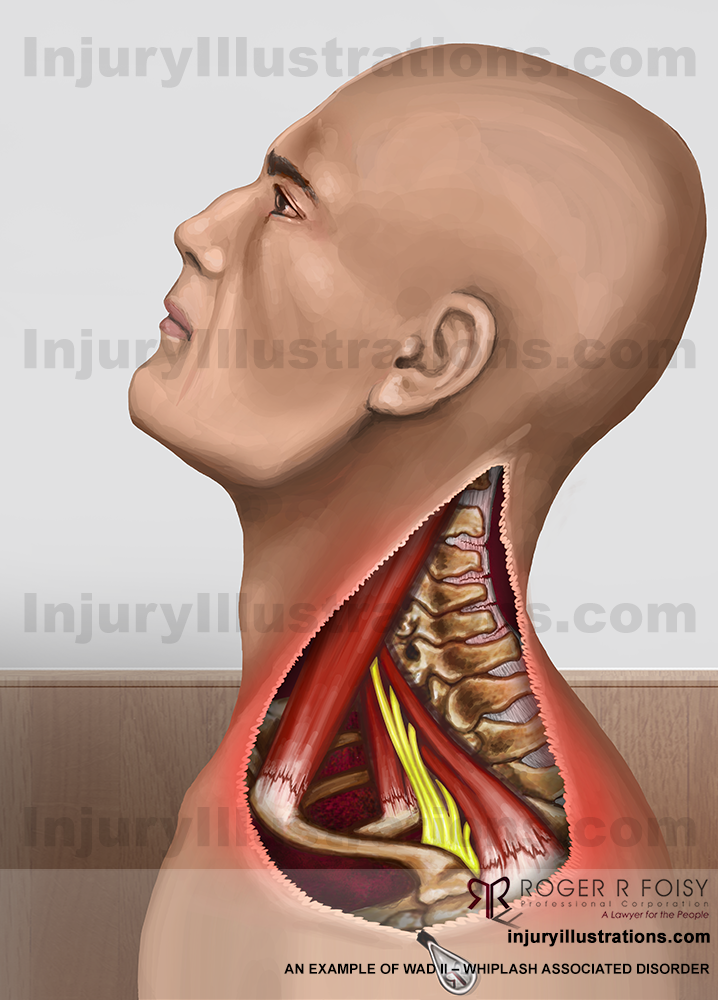
Potential Settlement: Whiplash Associated Disorder III
WAD III commonly results in decreased range of motion, decreased or absent deep tendon reflexes, muscle weakness, and sensory defects in the neck.
In 2007, the Court in Carrier v Wan, 2007 ABQB 279 awarded the injured person $60,000 for injuries that included WAD III.
To read the full decision, click here.
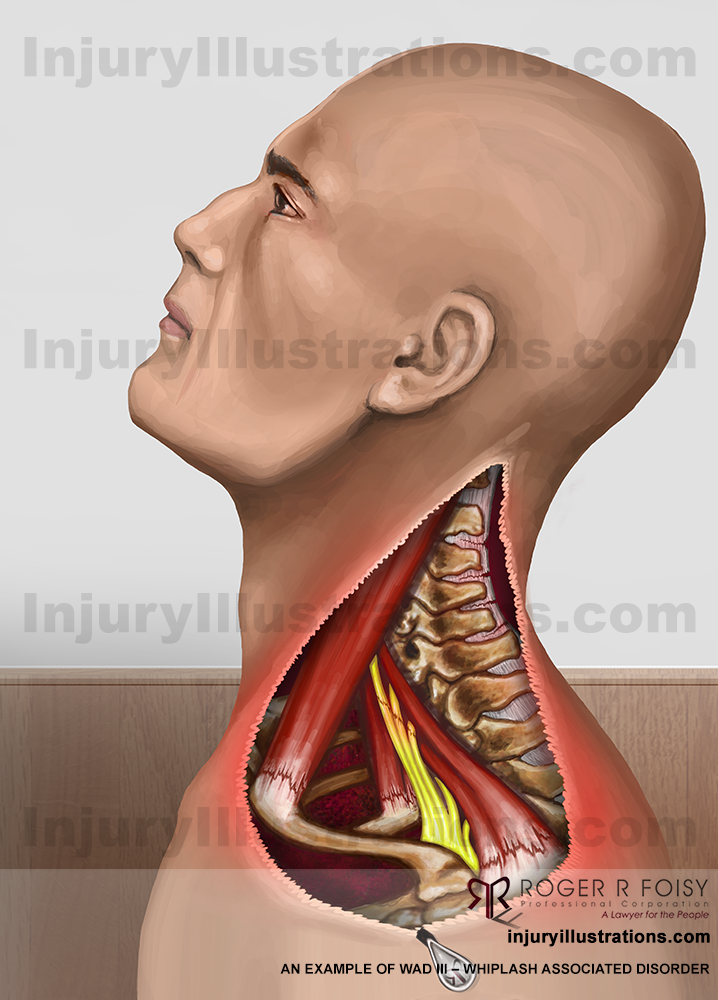
Potential Settlement: Whiplash Associated Disorder IV
WAD IV commonly results in a fracture or dislocation of the neck.
In 1993, the Court in Nagami v Larsen, 1993 CanLII 1268 (BC SC) awarded the injured person $85,000 for injuries that included WAD IV.
To read the full decision, click here.
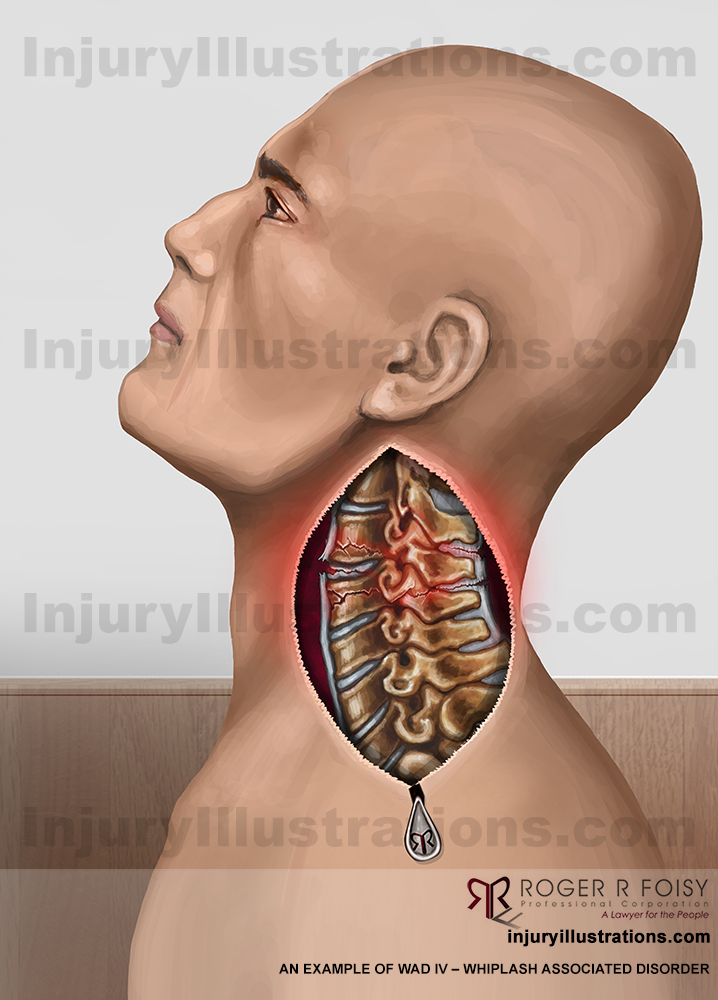
Receiving the Settlement You Deserve
People often believe that settlement value is mostly determined by the extent of the injury. While this is a factor, the most important information is how the injury has impacted your life. In other words, what does the injury prevent you from being able to do and how does this affect you?
A thorough lawyer should take the time to fully understand your specific situation, including your life and responsibilities before and after your accident, to ensure you do not under-settle your case. By quantifying every possible loss, you are more likely to receive a just settlement that will help to ease the financial burdens that usually occur during recovery.
If you have sustained a personal injury at another party’s fault, please contact me and my team of experienced personal injury lawyers for a free consultation.
Watch my video series about personal injury law.
More on Personal Injury from Roger R. Foisy:
Your Auto Insurance Coverage Has Been Cut Back
On June 1, 2016, auto insurance coverage in Ontario was changed. As of June 2017, all Ontario drivers will have renewed their auto insurance and will be on the new coverage.
Your new auto insurance makes cuts to coverages and increases the difficulty in qualifying for certain coverage in the event of an accident.
Insurance coverage for motor vehicle accident victims has been steadily reduced in Ontario since 1990. Even since just 2010, we’ve seen a rapid decline.
In fact, a recent report found that Ontario’s auto insurance system is “one of the least effective” in Canada. According to NDP deputy leader Jagmeet Singh, “Every change has systematically cut the coverage that Ontarians receive and benefited not the people but insurance companies.” Read more in the Toronto Star.
Here is a quick breakdown of the auto insurance coverage we’ve lost since 2010:
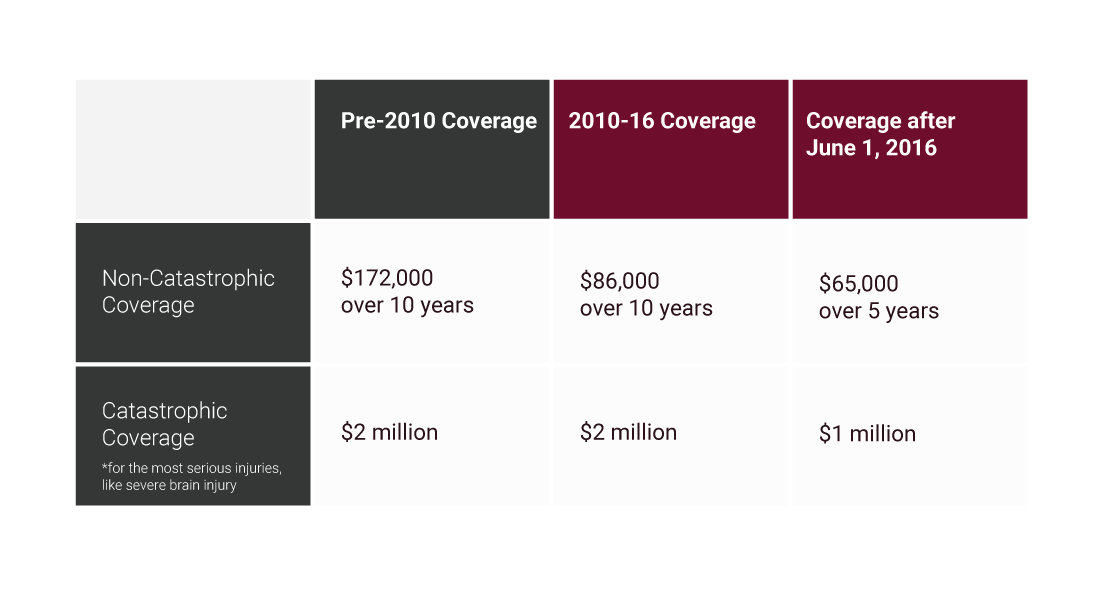
If you didn’t purchase optional increases to your coverage when your auto insurance policy renewed between June 2016 and July 2017, your coverage will have been significantly cut back.
As a personal injury lawyer, I can confidently say that these reduced benefits are highly unlikely to be sufficient to cover your medical, rehabilitation, and attendant care costs if you are seriously injured in a motor vehicle accident.
What Can You Do?
I highly recommend purchasing additional coverage in your auto insurance policy. Do not rely on your auto insurance company to have your best interests at heart; TAKE STEPS TO PROTECT YOU AND YOUR FAMILY. It’s very affordable and can make a substantial difference in the event you are involved in a motor vehicle accident.
I’ve put together this infographic to showcase this issue. I encourage you to share it with other Ontario drivers:
No Title
No Description
Every Ontario driver needs to know about these recent cuts to their coverage and understand the value of the optional benefits available to them.
I also encourage readers to view these additional resources for more information about auto insurance in Ontario:
- “Optional Benefits Are Now Less “Optional” Than Ever” by the Ontario Trial Lawyers Association
- Information about changes to auto insurance from the Financial Services Commission of Ontario
- The Truth About Insurance informational website by the Ontario Trial Lawyers Association
Roger R. Foisy is an Ontario Personal Injury Lawyer with extensive experience in motor vehicle accident cases. If you or a loved one have been injured in a motor vehicle accident, please contact us for immediate support and a free consultation.
Watch my personal injury video series.
More on Motor Vehicle Accidents from Roger R. Foisy:
Personal Injury Potential Settlement Values: Temporomandibular Joint (TMJ) Injury
TMJ injuries involve pain and dysfunction of the muscles that move the jaw and the joints which connect the jawbone to the skull. Some causes include injury to the teeth, jaw, or arthritis.
In this article, we will take a look at two TMJ injuries and historical examples of the personal injury settlement values victims have received:
(more…)
New Resource! Personal Injury Potential Settlement Values
I am excited to announce the launch of a new educational section of my website: Illustrations of Common Injuries & Potential Settlement Values.
This resource offers injury information and settlement examples for a large number of common personal injuries. Each injury has a unique page that includes:
10 Ways Employers Help Prevent Employees from Developing Psychological Long Term Disabilities [Infographic]
A good workplace can help reduce the anxiety and stress that often leads to a psychological long term disability claim.
Although every mental illness is unique to the specific individual and circumstances, I have some general tips for employers to take proactive steps in making the workplace a better environment for everyone:
(more…)
Personal Injury Potential Settlement Values: Mild Traumatic Brain Injury and Concussions
Brain injuries are classified as mild, moderate, or severe. The leading causes are vehicle-related collisions, falls, sports injuries, and assaults. Of these brain injuries, 70-90% are considered “mild” and are commonly referred to as “concussions”. It is important to realize, however, that there is nothing mild about a traumatic brain injury.
(more…)
Educational Long-term Disability Resources
At the Roger R. Foisy injury law firm, we strongly believe in educating people as much as possible about the process of injury and long-term disability (LTD) law in Ontario, as well as helping them understand what to do and what to expect after an injury or disability.
In pursuit of this goal, we’ve built up numerous resources including videos, infographics, FAQs, and more.
Riskier Roads – GTA Pedestrians and Cyclists Being Run Down at Record Rates
A rash of pedestrian and cyclist accidents in the GTA has been alarming to those people who choose to walk or bicycle. It is particularly upsetting because these accidents have caused increased pedestrian fatalities.
With the continual increase in the number of automobiles in Ontario coupled with a rise in the number of inexperienced or inattentive drivers, we are seeing a marked upsurge in the number of pedestrians and cyclists struck by cars, vans, and trucks.
(more…)
How the Possible Upcoming Legalization of Marijuana May Affect Medical Marijuana Users
Currently, the possession, distribution, and production of marijuana is illegal in Canada except for certain medicinal uses (studies show it can be effective to treat conditions including chronic pain, PTSD, and depression). However, in spring 2017 the Canadian federal government is expected to legalize marijuana for recreational use.
The Ontario Trial Lawyers Association (OTLA) has published a blog addressing this topic, with particular attention to the current process for individuals to acquire medical marijuana and how the legalization could affect both those who use it for medical purposes and the general public.
(more…)
Some Do, We Don’t – Roger R. Foisy Addresses Toronto Star Article
 A Condemnation of Ontario Injury Lawyers Charging Unjust Fees
A Condemnation of Ontario Injury Lawyers Charging Unjust Fees
On Saturday, the Toronto Star published an investigative article titled “Double-dipping lawyers taking big slice of injury settlements”. The article details the practice of some Ontario Personal Injury Law Firms of charging a contingency fee (“we only get paid if you win”) and taking a second fee on top of that called “costs”.
This has never been a policy at my firm and, as I outlined in one of my client-friendly videos in 2012, this practice has been disallowed by the Ontario Solicitors Act because it leaves personal injury claimants with less money in their pocket at the end of a settlement. I am firmly against this practice, and believe that all law firms in Ontario currently engaging in such a practice must stop.
(more…)
10 Things Employers Can Do to Accommodate Employees with Physical Long Term Disabilities [Infographic]
Ontario employers have a legal duty to accommodate employees with long term disabilities who are returning to work.
Although accommodations must be made based on the specific individual and their particular disability and circumstances, I have some general tips for employers seeking to properly accommodate individuals with physical disabilities:
(more…)
New Concussion Blood Test Developed with a 90% Accuracy Rate!
Last week, the Globe and Mail reported that researchers at Western University in London, Ontario have developed a new blood test to assess whether an individual has suffered a concussion – and the test has an amazingly high accuracy rate of 90%!
that researchers at Western University in London, Ontario have developed a new blood test to assess whether an individual has suffered a concussion – and the test has an amazingly high accuracy rate of 90%!
The results are still preliminary, with a small test size of 12 concussed male athletes and 17 non-concussed male athletes; however, the results are convincing and have been published in the peer-reviewed medical journal Metabolomics.
If this test is validated through further study, it could make a significant difference for people who have suffered a concussion. Concussions and other brain injuries have often been called the “invisible disability” because they are typically not physically apparent and are difficult to accurately test for. An accurate blood test for concussions would provide the patient and medical professionals with concrete evidence of the injury. This would make it easier for medical practitioners to know when to treat for concussions and – critically – for individuals to know when they need to be extra cautious.
(more…)
Merry Christmas from the Roger R Foisy Law Firm!
 Merry Christmas and a happy New Year from the team at Roger R Foisy! We wish you a joyful holiday season with your loved ones.
Merry Christmas and a happy New Year from the team at Roger R Foisy! We wish you a joyful holiday season with your loved ones.
Our Holiday Hours
December 24 – 27: Closed
December 28 – 30: Open
January 2: Closed
January 3: Open
(more…)
How Speech-Language Pathologists Help Traumatic Brain Injury Victims
 In my previous video (and blog) about finding the right team for your brain injury rehabilitation, one of the key specialists I mention is the speech-language pathologist.
In my previous video (and blog) about finding the right team for your brain injury rehabilitation, one of the key specialists I mention is the speech-language pathologist.
A speech-language pathologist is a medical professional who specializes in speech disorders and cognitive-communicative disorders. According to OSLA (Ontario Association of Speech-Language Pathologists and Audiologists), over 75% of individuals with acquired brain injury (ABI) experience difficulty with various aspects of speech and communication. These difficulties are typically cognitive-communication impairments that can impact their ability to return to work or school, as well as relationships with family and others in their lives.
New Auto Insurance Rules Reduce Rehabilitation Payout for Victim with Traumatic Brain Injury
 I have blogged frequently in the past few years about the reduction of auto insurance benefits in Ontario and how these changes are hurting car accident victims. In my last blog, I recommended Ontario drivers consider adding optional benefits to their insurance for this reason.
I have blogged frequently in the past few years about the reduction of auto insurance benefits in Ontario and how these changes are hurting car accident victims. In my last blog, I recommended Ontario drivers consider adding optional benefits to their insurance for this reason.
Ontario Drivers: Do You Know about These Recent Reductions to Your Auto Insurance Coverage?
 Did you know your auto insurance benefits were reduced on June 1, 2016?
Did you know your auto insurance benefits were reduced on June 1, 2016?
I have found many of my motor vehicle accident (MVA) personal injury clients are not aware of the recent changes to automobile insurance; I am writing this article because it is very important for every Ontario driver to know about them, as optional benefits are available that will ensure you are covered in the case of a collision.
(more…)
What Happens During the Mediation of a Personal Injury Claim? [Video]
Statistics show that 97% of personal injury cases settle before going to trial. One of the most effective ways to settle a claim is during mediation, which can result in a fair settlement of your case without needing to go to trial.
(more…)
Driving Rehabilitation Services after Personal Injury
 What Are Driving Rehabilitation Services?
What Are Driving Rehabilitation Services?
Driving rehabilitation is a service for personal injury clients who need assistance to get back into their vehicle and on the road to recovery. Similar to driver’s education courses, it involves a combination of rehabilitative activities inside the car and outside of the car. Clients are introduced to strategies for how to drive under the new circumstances they are now faced with. (more…)
Helping Children Overcome Psychological Trauma after Car Accidents
 A motor vehicle collision is a traumatic experience for everyone involved. The psychological effects of such an accident can last for a long time, regardless of age, whether you were the driver or passenger, or whether you were physically injured or not. (more…)
A motor vehicle collision is a traumatic experience for everyone involved. The psychological effects of such an accident can last for a long time, regardless of age, whether you were the driver or passenger, or whether you were physically injured or not. (more…)
Quantifying Damages: Personal and Attendant Care
After suffering a personal injury from an at-fault party, victims are entitled to compensation for the serious injury and any resulting disability. A personal injury lawyer fights to secure the maximum settlement for their injured client, based on their ability to demonstrate the extent of the “damages” the person sustained across all facets of their life (work, home, social, etc.). (more…)
Quantifying Damages: Housekeeping and Home Maintenance
After suffering a personal injury from an at-fault party, victims are entitled to compensation for the serious injury and any resulting disability. A personal injury lawyer fights to secure the maximum settlement for their injured client, based on their ability to demonstrate the extent of the “damages” the person sustained across all facets of their life (work, home, social, etc.).
Congratulations to Stephanie Weir for Being Called to the Bar!
We are excited to announce our staff member Stephanie Weir was called to the bar on June 20, 2016. Stephanie started with the firm as a Law Student in 2012 and we are proud of her and her achievements! (more…)
It’s the Law! Cyclists under 18 Must Wear Helmets
Did you know that from 2006 to 2010, 93.75% of cyclists under the age of 18 who were killed in cycling collisions were not wearing a helmet? (The Ontario Ministry of Health) (more…)
Preparing for an Insurance Company Independent Medical Examination [Video]
Personal injury clients are often asked to undergo an Independent Medical Examination (IME). These evaluations are common practice when you are engaged in a personal injury or long-term disability claim. (more…)
May Is National Fitness Month: Staying Healthy Can Help Your Recovery in the Case of Personal Injury
May is National Fitness and Sports Month, intended to encourage everyone to get active and take care of their bodies! As you are most likely already well aware, staying fit and healthy has a multitude of benefits, including increasing your protection from: (more…)
Seeking Compensation for a Compression Fracture of the Back
Throughout my years as an Ontario Personal Injury Lawyer, I have represented many clients with injuries that have included a compression fracture of the back (also referred to as a spinal compression fracture). Although this injury often heals with time, clients can claim various pecuniary (monetary) and non-pecuniary (non-monetary, such as pain and suffering) losses, depending on the circumstances of the injury.
Roger R. Foisy to Give a Presentation on Best Practices for Small Personal Injury Law Firms
With the help of my dedicated team, I have grown the Roger R. Foisy injury law firm from a small firm with only 4 client files in 2007 to a firm with about 75-80 cases at any given time by 2015. Growing much larger would not fit within my business model of providing a very personal level of attention to each and every client we take on.
Why You May Want to Consider Getting an Individual Disability Insurance Policy (Even If You’re on a Group Policy through Your Employer)
Many employers offer employees a group insurance policy as part of their compensation package; these policies typically provide some kind of long-term disability (LTD) coverage. I have written in the past about the importance of fully understanding your LTD policy, as well as understanding your policy’s specific definition of disability. (more…)
Uniquely Qualified: Personal Injury Lawyer Roger R. Foisy’s Medical Diplomas and Certificates
As a personal injury and long-term disability lawyer, I work with clients who have sustained a wide variety of injuries and illnesses. The more knowledgeable I am concerning medical topics and the human body, the better I am able to ensure my clients receive a fair settlement – one they truly deserve based on their specific injury or illness. (more…)
Alert for Ontario Drivers: New Road Safety Laws Passed to Protect Pedestrians
As of January 1, 2016, new road safety laws have passed in Ontario. It’s important for all drivers to be aware of these new laws, primarily to protect the safety of pedestrians and avoid motor vehicle accidents – but also to avoid new fines. (more…)
What Is the Settlement Value for My Injury or Illness? [Video]
As an Ontario Injury lawyer, one of the most common questions I’m asked is “What is the settlement value for my injury or illness?” (more…)
When Personal Injury Impacts an Elderly Person’s Mobility
Mobility is extremely important for our health and happiness as we age. Elderly people who are mobile are typically better able to retain their independence and stay active into the golden years. (more…)
Merry Christmas from the Roger R Foisy Team!
From everyone at Roger R Foisy’s personal injury law firm, Merry Christmas and a healthy New Year! We hope you can enjoy good company, good food, and good fun over this holiday season. (more…)
Suffering from a Whiplash Injury? You May Have a Brain Injury
As an Ontario personal injury lawyer with expertise in brain injury, I have helped many clients with injuries that were initially diagnosed as whiplash, but turned out to involve brain injury as well. That is why it is essential to always think ‘Brain First’. Unfortunately, these whiplash and brain injury victims can have trouble receiving the compensation they deserve and the treatment they need for their brain injuries. (more…)
Initial Client Interview: What Personal Injury Victims Can Expect [Video]
Typically, personal injury victims do not have experience with the legal process, and therefore do not know how to proceed after being injured. Of course, seeking medical attention should be your top priority. However, after seeking medical attention, you may wonder whether you will require legal representation. (more…)
Seeking Compensation for Coccyx or Sacral Fractures
As an Ontario personal injury lawyer, I have helped clients with a wide variety of injuries and illnesses receive the compensation they deserve. A coccyx or sacral fracture is not a common injury; however, it can have a large impact on a person’s ability to carry out their regular activities of living, including their ability to work. (more…)
Do You Understand the Definition of Disability in Your Group Insurance Policy?
I recently wrote about the importance of fully understanding your long term disability group insurance policy. If you do not understand your policy, you may find that you don’t receive as much compensation as you are expecting; or, you may fail to ensure that the records of your current salary are kept up to date, in which case you would not receive the full amount you are due. (more…)
How Parents Can Assist Children with Brain Injuries in Returning to School
Children who have experienced a traumatic brain injury (TBI), ranging from mild to severe, are more likely to face difficulties when returning to school after the incident or after a period of rehabilitation. (more…)
Why You Must Fully Understand Your Long Term Disability Group Insurance Policy [Case Study]
Misunderstanding your long term disability (LTD) group insurance policy can result in a great deal of stress if you are ever in a position to require those benefits. Unfortunately, your LTD policy may not be as straightforward as you think. (more…)
Roger R. Foisy Appointed to the Ontario Brain Injury Association Board of Directors
Over my years as an Ontario personal injury lawyer, I have seen the impact brain injury has had on many of my clients. Due to this, I have become a passionate advocate for brain injury awareness and I have completed courses from Brock University in Neurorehabilitation, Advanced Brain Injury Rehabilitation, Neurological Assessments: Beyond Testing to further my understanding of traumatic brain injury and recovery, and Children and Youth with Acquired Brain Injury. (more…)
Do You Know the Truth about Auto Insurance in Ontario?
I am continually disappointed by the ongoing changes to auto insurance in Ontario.
In two recent blogs, I have outlined recent major changes to auto insurance that are harmful to motor vehicle accident victims: (more…)
Ontario Trial Lawyers Association Against New Auto Insurance Regulations
My team and I recently attended an Ontario Trial Lawyers Association (OTLA) event, Driving for Success: Maximizing Your Auto Case.
Attended by over 500 OTLA members, the conference focused on a range of topics about auto insurance cases. The most important issue covered, in my opinion, is the new Ontario budget that effectively reduces benefits for motor vehicle accident (MVA) victims. (more…)
What Can I Expect at an Examination for Discovery? [Video]
My personal injury and insurance disability clients often have many questions about what to expect during the Examination for Discovery process. I would like to begin by emphasizing that although it is a serious matter, it does not have to be frightening. It’s okay to be nervous – but you will find once the process begins that it’s fairly relaxed. (more…)
There’s No Such Thing as “Just a Concussion”
Recently, an article in CBC News came to my attention about a 17 year old girl who ignored concussion symptoms, leading to her death.
I am always saddened by news like this. Especially when people ignore concussions because they think it’s “just a concussion”. It is never “just a concussion”. Concussions are mild traumatic brain injuries (mTBI); it’s as simple as that. (more…)
New Ontario Budget Sides with Auto Insurance Companies over Accident Victims … Again
The 2015 provincial budget was announced on April 23, claiming to bring adjustments and reforms to the Ontario auto insurance industry.
Initially, this sounds like a positive change. For the past 5 years, MPPs have passed bills regarding auto insurance that takes away their constituents’ rights. (more…)
Seeking Compensation for a Temporomandibular Joint (TMJ) Injury
As an Ontario personal injury lawyer, I have helped many clients with temporomandibular joint (TMJ) injuries receive the proper compensation. Through my years of experience, I have seen the serious impact TMJ injuries have on a person’s ability to carry on with their regular activities of living. (more…)
Myths and Facts about Child Brain Injuries [Infographic]
If you or a loved one sustains a traumatic brain injury – whether it is mild, moderate, or severe – it is a difficult time in your life. Brain injuries often require extensive rehabilitation, and can have long lasting effects. (more…)
How an Occupational Therapist Can Help Personal Injury Lawyers Achieve a Favourable Settlement
If you or a loved one sustains a serious injury as a result of negligence from another party, you may need to employ a personal injury lawyer. A personal injury lawyer works to ensure you receive proper compensation for your injury, including funds to support your resulting medical expenses and maintain your quality of life. (more…)
Dealing with Difficult People Workshop
I recently attended a 3 day workshop in Ottawa called “Dealing with Difficult People”.
The workshop is intended to help professionals improve their techniques and strategies for engaging in difficult conversations or dealing with difficult people. Having the skill and confidence to respond appropriately to these situations can lead to positive outcomes for all involved. (more…)
Bill 15: Changes to Ontario Auto Insurance Regulations Hurt Motor Vehicle Accident Victims
Bill 15, The Fighting Fraud and Reducing Automobile Insurance Rates Act, 2014, has recently passed in Ontario.
Ostensibly, the Bill’s purpose is to reduce automobile insurance fraud and reduce insurance premiums by 15% for drivers. (more…)
Insight from the 2015 Traumatic Brain Injury Conference in Toronto [Video]
On January 30, 2015, I will be attending the annual Traumatic Brain Injury Conference hosted by the University Health Network (UHN) Toronto Rehabilitation Institute. (more…)
Ontario Trial Lawyers Association 2015 Long Term Disability Conference
Today, January 23, 2015, I am attending the Ontario Trial Lawyers Association (OTLA) Long Term Disability Conference: Good Practices and Bad Faith From Coast to Coast. (more…)
How Employers Can Become a Cause of Long Term Disability Claims
As an Ontario Long Term Disability Lawyer, I have helped many clients settle long term disability (LTD) insurance claims. Through this experience, I have observed that the majority of my LTD clients are making claims due to disabilities related to the workplace. (more…)
Merry Christmas and a Happy New Year!
Roger R Foisy and his team of personal injury lawyers would like to wish everyone a Merry Christmas and a Happy New Year! (more…)
Seeking Compensation for a Knee Injury
As an experienced Ontario Personal Injury Lawyer, I have represented many clients suffering from knee injuries and have ensured that they received proper compensation. Like any injury that impacts mobility, knee injuries can have a far-reaching effect on a person’s regular activities of living, including their occupation, daily tasks, and recreational activities. (more…)
The Long Term Disability Insurance Process and Why It Can Fail
Many people with valid long term disability (LTD) claims are denied. Why does this happen?
Shouldn’t our system have processes in place to ensure that those who need long term disability receive it? (more…)
Seeking Compensation for a Basal Skull Fracture
In my experience as an Ontario Personal Injury Lawyer, I have assisted several clients with basal skull fractures and ensured that they received proper compensation. As the injury involves damage to the brain, a basal skull fracture can cause significant problems for victims in their daily lives.
What Is a Basal Skull Fracture?
Basal skull fractures are most often seen in motor vehicle accidents, slip and fall accidents, and – unfortunately – child abuse cases. (more…)
Why Insurance Companies May Have You Under Surveillance (And How You Can Lose Your Long Term Disability Compensation)
When you have made a claim for or are receiving long term disability insurance benefits, insurance companies will often look for reasons to deny or terminate your disability benefits. It is in their best interest to demonstrate that you are fit for work and do not require ongoing disability insurance for your condition. (more…)
Seeking Compensation for an Ankle Injury
Throughout my years as an Ontario Personal Injury Lawyer, I have helped many clients with ankle injuries receive proper compensation. Unfortunately, many people do not think an ankle injury is particularly serious; however, I have found that this type of injury can have a large impact on a person’s daily life. (more…)
Distracted Driving Causes Motor Vehicle Accidents
The Toronto Sun has published yet another saddening article about driving while distracted by a cell phone. It tells the story of a teen in 2009 who lost control of his car and died after reaching for a ringing phone. (more…)
Take the ‘Heads Up: Concussion in Youth Sports’ Free Online Training Course
We can often take it for granted that kids will get concussions when they play sports growing up. We think, “It’s just a concussion”. We brush it off.
Unfortunately, many people don’t know that a concussion is actually a mild traumatic brain injury (mTBI). Mild traumatic brain injuries can be quite serious and should not be taken lightly.
I encourage you to take the time to educate yourself about the potential risks of youth sports concussions: click here for a more in-depth discussion in my previous post, “What You Need to Know About Sports-related Injuries: Mild Traumatic Brain Injuries and Concussions”. (more…)
Long Term Disability: Why Is It Difficult to Receive Funding for Psychological Disabilities?
Long term disability (LTD) occurs when you are unable to work due to an injury or an illness. Those who suffer from injury or illness and have previously purchased disability insurance are able to submit an LTD claim through their disability insurer, which gives them a degree of financial security during this difficult time.
Compensating for the Emotional and Psychological Impact of Scar, Burn, and/or Disfigurement Injuries
Scar, burn, and disfigurement injuries are different from other types of injuries that I, as a personal injury lawyer in Ontario, help clients receive compensation for. My clients with these kinds of injuries experience psychological and emotional difficulties that are very distinct and do not materialize in the same was as in other cases.
It is important for the injured person to understand these psychological and emotional impacts, and to know that their feelings are valid and normal.
Don’t Neglect to Renew Your Driver’s Licence
Renewing your driver’s licence is a simple process – and it can save you from facing expensive insurance issues, should you get in an accident while your licence is expired.
No one ever thinks they will get into a motor vehicle accident, yet collisions happen every day. Even if you are a careful driver, you cannot always predict the behaviour of other drivers. You should never let your licence expire, in case of the unexpected.
(more…)
Coping with the Emotional and Psychological Impact of a Mild Traumatic Brain Injury [Video]
In my time as a Personal Injury Lawyer, I’ve worked with many clients that have suffered from a mild traumatic brain injury (mTBI). My clients often feel as though no one understands what they are going through. Sometimes, even they do not fully understand what is wrong.
This is because brain injury can often be seen as an “invisible disability”. Often, no outward injuries or wounds are present to give an external indication of injury. Unfortunately, this can mean others may not recognize or acknowledge the extent of your injury.
(more…)
Finding the Right Team for Your Mild Traumatic Brain Injury [Video]
When you have suffered a mild traumatic brain injury (mTBI), it is critical to have the right team of specialists at your side to help you through the rehabilitation process.
As I’ve mentioned previously, every brain injury is different depending on the location, combined effects, and severity of the damage. Therefore, the professionals you will need on your team may vary depending on your specific injury.
(more…)
Daily Court Information Now Available Online in Ontario
The Superior Court of Justice and Ontario Court of Justice have created a new online resource to make it easier for people to know when and where they need to go to court across Ontario.
This service publishes the daily court lists for these two bodies, including:
- Case name
- Names of those involved in the case
- Time
- Room number
- Reason for court appearance
Seeking Compensation for a Rotator Cuff Injury
Over my years as a personal injury lawyer in Ontario, I have helped many clients with rotator cuff injuries receive the proper compensation. Through this experience, I have seen how rotator cuff injuries can have a widespread impact on a person’s daily activities of living.
Trying to Access Your Own Medical Records in Ontario? Be Prepared to Pay.
Ontario residents are being charged excessive fees by pharmacies and medical offices simply to obtain their own medical records. Although this is a topic I have addressed before, it unfortunately continues to be an issue.
A recent article in the Toronto Sun by Alan Shanoff, “Our information, their files”, details the current problem we face. As he mentions, public officials have tabled this issue several times in past years, yet nothing has changed.
Fees range widely, often amounting to hundreds of dollars, as there are no laws to govern the charges.
Changes to Prejudgement Interest at the Expense of Motor Vehicle Accident Victims
The recent Bill 171 “Fighting Fraud and Reducing Automobile Insurance Rates Act” introduced by Ontario’s Minister of Finance, proposes reducing the amount of interest insurers must pay on compensation owed to motor vehicle accident (MVA) victims. Currently, the interest rate is 5%, but under Bill 171, the rate would become 1.3% and be modified quarterly.
This latest change was presented without notice or any consultation with any industry stakeholders.
As a recent article by Alan Shanoff of the Toronto Sun describes, this change is far from good for MVA victims.
Accessing Funding for Medical Rehabilitation after Suffering a Mild Traumatic Brain Injury in a Motor Vehicle Accident [Video]
If you, or a loved one, have been injured in a motor vehicle accident, it is important to understand the different levels of funding available to you. The funding you receive is dependent on the severity of your injuries; therefore, it is essential to recognize what your symptoms may mean so you can fight to obtain the appropriate funding.
It is critical to think “Brain First”. Mild traumatic brain injuries (mTBIs) are often missed because people attribute their symptoms to their more obvious injuries. It is only once the person has recovered from those injuries that their brain injury becomes more apparent. Knowing the symptoms can help you recognize the brain injury earlier on.
It is best to have a brain injury diagnosed from the beginning in order to receive the appropriate funding. With the right funding, your road to recovery will be financially supported.
Global Brain Awareness Week 2014
 This week, March 10-16 2014, is Brain Awareness Week (BAW). Through my experience as a personal injury lawyer, I know firsthand the importance of understanding the facts about brain injury.
This week, March 10-16 2014, is Brain Awareness Week (BAW). Through my experience as a personal injury lawyer, I know firsthand the importance of understanding the facts about brain injury.
I have created many educational resources about brain injury, including blogs, videos, a FAQ, and a glossary. I encourage everyone to check them out during BAW.
Videos
– What is a Mild Traumatic Brain Injury (mTBI)?
Sidewalk Disrepair Leads to $107,765 Settlement for Injured Woman
The Ontario Superior Court of Justice recently awarded a $107,765 settlement to Glenda Grayling following a fall on November 25, 2009 on a Caledonia city sidewalk.
Glenda and Kevin Grayling alleged that Mrs. Grayling’s fall was caused by the defendant’s negligence. The defendant in the case was The Corporation of the County of Haldimand, responsible for sidewalk maintenance at the time of the incident.
On November 25, 2009, Mrs. Grayling stubbed her toe due to the difference in height between two slabs of the Caledonia sidewalk. Doing so caused her to take several quick steps forward and fall on her right arm.
A small elevation difference between sidewalk slabs is not always considered “non-repair”, otherwise the city would be responsible for every pedestrian walking on the sidewalks. However, Haldimand County guidelines classify a sidewalk as hazardous if a “major” defect of over one inch exists.
Why are Mild Traumatic Brain Injuries Often Missed? [Video]
Mild traumatic brain injuries (mTBI) are often missed by both the injured person and medical practitioners.
In the following video, I explain the reasons why mild traumatic brain injury is typically overlooked:
1. After an accident causing injury, the most obvious physical injuries are prioritized.
For example, a pounding headache following a car accident may be attributed to a neck strain whiplash injury and upper back pain, rather than a brain injury. People fail to think “brain first”, dismissing symptoms of brain injury as side-effects from their more obvious injuries.
Furthermore, many healthcare providers do not specialize in brain injury and therefore may not recognize the severity of the brain injury.
5 Reasons Why Substance Abuse is Linked to Brain Injury
Substance abuse is the overindulgence in, compulsive use of, or dependence on drugs and/or alcohol, particularly to the point of interference with work, home, or social life.
Any substance use by an individual who has suffered from a traumatic brain injury (TBI), including a mild traumatic brain injury (mTBI), can have serious repercussions. It can make recovery times longer and symptoms worse, as well as interacting poorly with prescribed medications.
Yet, there are several connections between substance abuse and brain injury. The following are many of the reasons why you or your loved one may develop a substance abuse problem after suffering from a TBI:
Changes to Accident Benefits for Vehicle Collision Victims in Effect as of December 17, 2013
In December 2013, the government quietly passed regulations that change accident benefit insurance for motor vehicle collision victims. These alterations came into effect on December 17, 2013. Unfortunately, the changes are not to the benefit of those seeking personal care following an injury in a collision.
The modifications to the Statutory Accident Benefits will make it more difficult for an insured person who is injured in an auto accident to make a claim and receive an appropriate amount of benefits. The key area of the regulation that has been altered to create additional restrictions is attendant care benefits payable.
What is a Mild Traumatic Brain Injury (mTBI)? [Video]
Brain injuries are classified mild, moderate, or severe. The leading causes are vehicle-related collisions, falls, sports injuries, and assaults. Of these brain injuries, 70-90% are considered “mild”. It is important to realize, however, that there is nothing “mild” about a traumatic brain injury.
A brain injury, of any classification, must be taken very seriously. The brain is complex; any injury that causes a disruption of its normal functioning is a traumatic injury.
Unfortunately, many people do not realize that a concussion is a mild traumatic brain injury (mTBI). Because of this, mTBIs are often not fully recognized or properly prioritized.
An mTBI affects each person differently. The extent and combination of effects will vary depending on the areas of the brain involved and the individual person.
Life Changes: Living with a Loved One Suffering from an mTBI

Mild traumatic brain injury (mTBI) does not only affect those who suffer the injury. That said, of course the person who is injured will be extremely impacted by the injury; however, it is important to realize that the lives of their close friends and family will also be changed.
If you are a loved one of someone who is suffering from an mTBI, you will likely go through difficulties as you struggle to accept the injury, your new situation, and the new person who has replaced the person you knew before the injury.
Common Emotional Reponses
There is a range of emotions that you may go through as you cope after someone you love has sustained a brain injury.
Using the PQRST to Accurately Describe Pain to Your Doctor [Video]
It is very important to effectively describe the pain you feel to your doctor. Without an accurate description, reporting that you are experiencing “pain” will not help the doctor assess your condition.
Furthermore, a vague description does not properly convey how your pain is affecting your ability to function and work. The information you provide to your doctors is used to create reports for the insurance companies. These reports give credibility to your claims. This is why it is essential to fully explain the impact of your injuries, the extent of your pain, and how your daily function has been affected.
You should use the PQRST Method as a tool to help you accurately describe your pain to healthcare practitioners.
A Silent Epidemic: Minor Traumatic Brain Injury – Science Daily
 A recent article in Science Daily outlines a literature review from the Journal of the American Academy of Orthopaedic Surgeons (JAAOS) that focuses on mild traumatic brain injury (mTBI) as a common, but often overlooked, condition.
A recent article in Science Daily outlines a literature review from the Journal of the American Academy of Orthopaedic Surgeons (JAAOS) that focuses on mild traumatic brain injury (mTBI) as a common, but often overlooked, condition.
The study was based in the U.S., but I think that Canadians will find the information relevant as well. It is important to educate ourselves on the prevalence of this “silent epidemic”.
“In the United States, approximately 1.4 million people suffer a traumatic brain injury (TBI) each year. Of those injuries, three out of four are minor TBI (mTBI) — a head injury that causes a temporary change in mental status including confusion, an altered level of consciousness, or perceptual or behavioral impairments.”
How to Cope with Grief after Brain Injury
 Brain injuries, even those classified as “mild” traumatic brain injuries (mTBI), can have significant short and long-term impacts on the injured person’s life and the lives of their loved ones.
Brain injuries, even those classified as “mild” traumatic brain injuries (mTBI), can have significant short and long-term impacts on the injured person’s life and the lives of their loved ones.
It is completely normal and healthy to find yourself grieving after you or someone you are close to suffers from a brain injury. Grief and mourning are natural, important emotions. It is how we heal and are able to move forward after a loss. We grieve after events such as death, divorce, illness/injury, or even life transitions.
Brain injuries come with many losses. The person with the injury may have difficulties with day-to-day activities, a change in personality, or an inability to handle the demands of work. The challenges and changes can alter lifestyle, physical abilities, emotional capacity, financial independence, and social interactions. Grief is a common way to respond to these major changes and losses.
Although grief is different for everyone, some of the emotions you may experience include:
The Next Five Reasons an Insurance Company Will Deny Your Long-Term Disability Claim [Video]
In our previous video, we explained the first five reasons why an insurance company might deny your long-term disability claim or terminate your benefits. Click here to see it.
Today, our video is concerned with the next five common reasons why insurance companies deny long-term disability claims. If you are unable to work because of an injury or illness, it is crucial to be aware of the reasons why insurance companies deny claims.
1. Objective Evidence or Insufficient Information
If a claim for long-term disability benefits has little or no objective evidence and/or insufficient medical information to support the disability, it will be denied. Therefore, it is important to precisely describe how your injury or illness impacts your daily activities when seeing your doctor or specialist.
Evidence may include lab results, consultation reports, MRIs, ECGs, psychological assessments, etc.
2. Treatment and Assessment Compliance
You must be under medical care and comply with the rehabilitation program for your disability. This means regularly attending doctor appointments, seeing recommended specialists, and taking medication as prescribed. Failure to demonstrate compliance with your treatment will result in a denied claim or the termination of your benefits.
3. Contradictory Surveillance
Back to School – In Case of Emergency Program
 School will begin once again in September, and many parents worry about what will happen if their child is injured on the daily travel to and from school – particularly when the child is not accompanied by an adult.
School will begin once again in September, and many parents worry about what will happen if their child is injured on the daily travel to and from school – particularly when the child is not accompanied by an adult.
Unfortunately, accidents are a part of day-to-day life. Being prepared can make the difference in an emergency situation.
This is why we offer the In Case of Emergency (ICE) program. ICE is a term that is internationally recognized by emergency responders. An ICE card has the name and phone number of two emergency contacts, which the first responders can use to quickly reach the injured person’s immediate family.
The First Five Reasons an Insurance Company Will Deny Your Long-Term Disability Claim [Video]
If you are not able to work due to an injury or an illness, it is very important for you to be aware of the main reasons why an insurance company may deny your long-term disability claim. With knowledge of the five most common reasons why claims are denied, you may be able to avoid making mistakes that could cost you your long-term disability benefits.
1. Clerical or Procedural Errors
If anyone involved with your disability claim – the insured person, doctor, or lawyer – does not send all of the required documentation to the insurance company in a timely manner, you may be denied. Furthermore, there are statutory limitation periods that define the allowable amount of time between completing an insurance claim and filing for a lawsuit. After this period, you may be prevented from claiming disability benefits.
2. Having Pre-existing Medical Conditions
If you have a pre-existing medical condition before becoming insured, most private disability insurance policies (it must be noted that these are different than employee group policies) will require an exclusion of benefits related to the particular pre-existing condition for defined period of time.
3. Committing Fraud or Misrepresentation
Causes and Effects of Acquired Brain Injury [Infographic]
As an invisible condition, so few people are aware of the facts about acquired and traumatic brain injury. We have created this infographic to help highlight some of the causes and effects of this condition. We hope this resource will spark further discussion about this complex topic.
The Human Brain and Traumatic Brain Injury [Video]
The following video from brainstreams.ca – an online resource for Canadians dealing with brain injuries and their loved ones – is an excellent overview of the importance of brain injury awareness. This brief, 1 minute video teaches us that there are 165 000 brain injuries in Canada every year, 6 500 of which permanently disable those who suffer from them. The first step to understanding and supporting people with this condition is awareness.
In the spirit of National Brain Injury Awareness Month, please take a moment to watch the video and share it with others.
>> If you or a loved one has suffered a brain injury as the result of an accident or vehicle collision in Ontario, you can seek the help of an experienced personal injury lawyer to help ease the financial burden. Contact us for immediate support and a free consultation.
What Are the Symptoms and Effects of a Traumatic Brain Injury?
 If you or a loved one has recently been in an accident and suffered a traumatic brain injury (TBI) as a result, you may not know what to expect. It is particularly difficult to predict because no two brain injuries are the same.
If you or a loved one has recently been in an accident and suffered a traumatic brain injury (TBI) as a result, you may not know what to expect. It is particularly difficult to predict because no two brain injuries are the same.
The signs and symptoms of a TBI can be subtle. In fact, the symptoms may not appear for several days or weeks after the original injury. The true extent of the effects may not be apparent for some time.
When a brain injury occurs, the functioning of a variety of components of the brain can be affected. Since the brain is so complex, the particulars of the injury will determine which symptoms manifest.
The brain regulates the function of the rest of the body, and therefore the impact of a TBI is not limited to the brain. The changes can be temporary or permanent, and can result in ongoing impairment or the inability to perform certain tasks.
June is National Brain Injury Awareness Month in Canada
The Brain Injury Association of Canada (BIAC) has chosen June as National Brain Injury Awareness month. As with America’s brain injury awareness month, which took place in March, June is a time to educate ourselves on brain injury.
Resulting from a blow to the head or penetrating injury (e.g. gunshot wound), acquired brain injury has been called an invisible condition. This is because many of the symptoms and changes in the person with a brain injury are emotional and cognitive. Often, no physical evidence of the injury remains, leading others to assume the person is “fine”.
The leading causes of brain injury in Canada are automobile collisions, falls, pedestrian struck by vehicle, assault, cycling incidents, and sports injuries. Illnesses affecting the brain can also cause the same effects as an injury resulting from impact. As of 2012, close to 5.5 million Canadians were living with a brain injury, disease, or disorder. In Canada, brain injury is the premier cause of death and disability in people under 44. Yet, we hardly hear about it. That is why brain injury awareness month exists.
Fatal Accidents and Understanding Grief [video]
Losing a loved one in an unexpected circumstance, such as a vehicle accident, is extremely difficult. People who were close to the deceased often wonder why their grief seems to feel so much more potent when someone else is to blame for the accident. Tragic, unexpected events are more shocking and devastating than an illness or natural occurrence because they are sudden and impossible to anticipate.
Feelings of powerlessness and vulnerability are normal in this situation, and these types of catastrophic events can threaten our emotional security. Everyday tasks may become difficult as both the mind and body struggle to react to the inner turmoil of grieving for a loved one.
Strong painful emotions can be triggered by many things after the incident, including memories during significant festive events or family milestones. For those who were present during the accident, (for example, a passenger in the car), certain sounds, images, or scenarios may become triggers.
As discussed in a previous video, which you can click here to see, it is absolutely essential to take care of yourself during this difficult period of grief. Reach out to others for support; they can share the grief and lessen your burden.
When a loved one is lost, the future may seem uncertain and daily cares may suddenly feel overwhelming and insurmountable. The Ontario Court of Appeal recognizes that when fatal accidents occur and someone else is to blame, there must be financial consideration for the family members.
Preventing Child Injury: National Summer Safety Week
 The Canadian Safety Council has designated May 1st – 7th as National Summer Safety Week. It’s the perfect opportunity to strive toward child injury prevention and educate ourselves about safety.
The Canadian Safety Council has designated May 1st – 7th as National Summer Safety Week. It’s the perfect opportunity to strive toward child injury prevention and educate ourselves about safety.
The unfortunate reality is that injury is the leading cause of death for children in Canada, with an estimated 340 fatalities each year for ages 14 and under. An additional 25 500 children are hospitalized. Therefore, it is crucial that adults – parents, educators, guardians, community leaders, etc. – take the time to familiarize themselves with effective safety practices and programs.
The Canadian Safety Council has provided a good resource with tips for child safety, including bicycle safety, traffic safety, playground safety, and more. Ensuring that helmets are worn at all times when biking, and monitoring small children around water are just some of the ways that serious accidents can be prevented. Furthermore, simply teaching children about safety can help them to make smarter choices when they are in potentially dangerous situations.
Coping with Grief from the Loss of a Loved One [video]
Coping with the loss of a loved one can be one of the most difficult things that any of us have to go through in our lives. Particularly in the case of fatal accidents, when the loss is unexpected.
Our video today is a brief departure from issues of law, as we think it is important to provide help to those dealing with loss. Managing grief can be overwhelming, but it is essential to understand that the feelings you are experiencing are crucial for coping and for eventually finding closure. Grieving is a natural part of the healing process.
Experiencing a variety of emotions is normal and inevitable when coping with grief; feelings of sadness, regret, denial, anger, guilt, confusion, anxiousness, helplessness, loneliness, and isolation are all to be expected and accepted as part of the grieving process.
Grief manifests in both emotional and physical symptoms. Physically, it is completely normal to feel fatigued, lethargic, unable to sleep, and achy. Fluctuations in weight are also normal.
Once these emotional and physical symptoms are understood as part of the grieving process, they can be endured with patience. Self-blame and avoiding your emotions are destructive in these situations; if you are coping with grief, your priority must be to take care of yourself.
March is Brain Injury Awareness Month
 March has been designated brain injury awareness month by the Brain Injury Association of America (BIAA).
March has been designated brain injury awareness month by the Brain Injury Association of America (BIAA).
Brain injuries can affect a person’s cognitive abilities, emotional responses, and overall personality. Traumatic brain injury (TBI) can result when a person experiences a blow to the head, or from a penetrating injury (for example, a gunshot wound).
TBI is the leading cause of death and disability worldwide. According to Brain Injury Centre Canada, TBI is sustained by: 1) Falls (35.2% – often experienced by children and the elderly); 2) Traffic Collisions (17.3%); 3) Struck By/Against Events (16.5% – including many workplace accidents); 4) Assaults (10%); and Other/Unknown Incidents (21%).
What You Need to Know about Fatal Accident Claims [video]
What do you need to know about fatal accident claims?
The loss of a loved one is devastating, and the thought of pursuing legal action in a time of grief may seem intimidating. Although no amount of compensation can begin to make up for your loss, knowing your legal options can help to make the process a little easier.
The law recognizes the significant position held by the deceased. An experienced lawyer will be able to emphasize the strength and importance of the relationship with the deceased, in order to properly convey the depth of your loss.
What is Long Term Disability Insurance? [Video]
What is long term disability insurance?
Many people aren’t aware of their options when faced with a long term injury or illness. Insurance companies have rules and regulations which make it difficult to navigate through the claims process, and time limitations can block legitimate claims. It is important to understand your options.
In comparison to short term disability insurance, long term disability insurance is more permanent. It will reduce the financial hardship experienced by you and your family in the event that you are unable to return to work due to a medical condition. Most policies provide benefits for the first two years, but to qualify beyond that, you must be unable to perform the tasks required for any occupation that you are reasonably qualified for.
It is also important to note that you can obtain disability benefits even if your injury or illness occurred outside of the workplace. In this way, disability benefits differ from workplace-insurance benefits.
Highway 401 Multi-Vehicle Collision 2013
Last Friday, January 25, 2013, Southern Ontario experienced a multi-vehicle accident on the 401 near Newcastle.
As the busiest highway in North America, the 401 can become dangerous in poor weather conditions – such as the snow on Friday afternoon. The high volume of traffic, the slippery road conditions, and the poor visibility work together to compound the effect of a collision until it involves dozens of vehicles.
We are thankful that this recent pileup did not result in any fatalities. Of the five people who were injured, two were in serious condition. Fortunately, none of the injuries were life-threatening.
We are familiar with the challenges that face those involved in multi-vehicle collisions like this. In 1999, a similar incident on the 401 caused by a thick fog resulted in 8 motor vehicle accident deaths and 33 injuries. Having represented several families who were involved in this incident, we understand how difficult it can be.
It is a complicated situation, due to the sheer number of factors, vehicles, and people. There are no easy answers, and no simple solution.
There are a few things that we can all do to try to prevent accidents like this from happening in the first place. We can be respectful, courteous drivers; tailgating, cutting other drivers off, and refusing to let other drivers merge are all examples of dangerous behavior that contributes to collisions. Slow down when weather conditions are bad. Wear your seatbelt.
These are the simple things that can avert collisions and save lives. As we continue through this winter, we should make every effort to be safe on the road.
>> If you or a family member are a victim of a serious vehicle accident in Ontario, you need to seek the help of a dedicated personal injury lawyer. Contact us today for immediate support and a free consultation.
A Meaningful Book for Beginning the Healing Process
 Because we have grieving clients who have suffered the devastating loss of a loved one, we have begun to provide complimentary copies of this helpful book, I Wasn’t Ready to Say Goodbye by Brook Noel and Pamela D. Blair, PhD.
Because we have grieving clients who have suffered the devastating loss of a loved one, we have begun to provide complimentary copies of this helpful book, I Wasn’t Ready to Say Goodbye by Brook Noel and Pamela D. Blair, PhD.
Highly Readable and Sensitively Written
The twenty-four chapter book contains much helpful information and advice that is personable and conversational, highly readable and sensitively written. The authors importantly acknowledge at the outset that no one can “explain the impact of tragic death who has not experienced it firsthand.”
The book was written, they say, to provide light for those who are undergoing the “questioning, the disorientation, [and] the helplessness that arises.”
The Increasing Relevance of Social Media in FSCO Arbitration
A 2012 appeal decision by the Financial Services Commission of Ontario (FSCO) confirms that Facebook can be damaging to motor vehicle accident insurance claims. This appeal confirms an earlier decision that limited access Facebook photographs are relevant in assessing accident benefits claims.
In 2008, Eniko Rakosi was injured in a motor vehicle accident and applied for statutory accident benefits from her insurer, State Farm. There ensued disagreement regarding her entitlement to attendant-care, income-replacement, and medical benefits. Rakosi applied to FSCO for arbitration. (more…)
Pedestrian Death Review Calls for Pedestrian-Friendly Roads
After 95 pedestrian deaths in 2010, Ontario’s Chief Coroner undertook a Pedestrian Death Review in order to make recommendations for improved road safety. The review is clear that drivers of motor vehicles are not solely to blame. Pedestrian behaviour and unaccommodating road design also contribute to road safety.
70% of the deaths were attributable to five circumstances:
(1) Pedestrians struck at mid-block crossings (31%);
(2) Pedestrians struck on the sidewalk or a road’s shoulder (14%);
(3) Pedestrians struck without right-of-way in an intersection (11%);
(4) Pedestrians struck with right-of-way in an intersection by left-turning vehicles (7%);
Insurance Arbitrator Awards Medical Marijuana
The Financial Services Commission of Ontario has awarded a catastrophically injured motor-vehicle accident victim medical benefits for the purchase of medical marijuana. The victim’s insurance company is to make payments of $567.60 per month.
In 2000, the applicant suffered a major head injury. After being awarded and denied various accident benefits, she engaged her insurance company in mediation, which failed, and she then applied to FSCO for arbitration.
The applicant’s claim stated that prescription drugs, opiates, anti-depressants, tranquilizers, and hypnotic medications were ineffective. The victim claimed that marijuana was the only substance that alleviated her pain, anxiety, insomnia, and poor appetite without significant side effects.
B.C. Court Rules that Private Facebook Photos to be Disclosed in Personal Injury Case
The British Columbia Supreme Court declared that Facebook photos of the accident victim vacationing and playing sports must be handed over in order to better evaluate her personal injury claim stemming from a motor vehicle accident.
After a 2008 motor vehicle accident in which Tamara Fric sustained injuries including chronic severe headaches, injury and pain to the upper back and neck, she is suing for damages. Fric claims that the injuries caused by the accident resulted in a loss of the amenities of life, a loss of earning capacity and a loss of mobility among other things.
Maximum Attendant-Care Benefit not Limited to Extent of Economic Loss
When in a motor vehicle accident, regardless of fault, you are entitled to accident benefits from your insurance company. One benefit is for ‘attendant care,’ which covers daily-care expenses if you are no longer able to care for yourself.
The amount of attendant-care benefits depends on the seriousness of the injury. For serious or ‘catastrophic’ injuries—like quadriplegia, paraplegia, amputation, blindness, and brain injuries—the maximum attendant-care benefit is $1,000,000 for life (maximum of $6,000/month). It is essential to obtain appropriate financial support when coping with a serious injury. Frequently, this care comes from family members who take time from work to care for the injured person.
Understanding Your Legal Options for Accidental Injuries in Ontario [video]
[Video Below]
It is important to know what your legal options are if you have been injured in an accident in Ontario.
There is a potential case for a lawsuit for virtually anything, so you should ask yourself if it makes sense to start a lawsuit.
This should really depend on the severity of your injury and the impact the accident has had on your life
In some cases of minor injuries, such as a small cut or an injured toe, it may not make sense to retain an Ontario injury lawyer. A better option would be small claims court, which is available to individuals who may want to make claims under $25,000. You also have the option to hire a paralegal.
Introducing our ICE Program
 Accidents and illness are an unfortunate reality of our daily life. Being prepared in the event of an accident or sudden illness, such as a car accident or heart attack, will allow first responders to make the best of a difficult situation. As part of our on-going commitment to the local community, Roger R. Foisy Professional Corporation has developed a program to offer complimentary ICE (In Case Of Emergency) cards.
Accidents and illness are an unfortunate reality of our daily life. Being prepared in the event of an accident or sudden illness, such as a car accident or heart attack, will allow first responders to make the best of a difficult situation. As part of our on-going commitment to the local community, Roger R. Foisy Professional Corporation has developed a program to offer complimentary ICE (In Case Of Emergency) cards.
(more…)
School Bus Driver that Hits Child is not Found Negligent
As children start heading back to school it is beneficial to reflect on the issue of road safety. While children may act and play as though they are invincible they most certainly are not. Whether children walk to school, get a ride or take the bus there is still a risk. For all parents it is worth sitting down to have a talk.
Combining Physical and Psychological Impairments in Catastrophic Impairment
If suffering serious injuries from an accident, the method for assessing catastrophic impairment should be more inclusive according to an Ontario Court of Appeal decision. An assessment of physical and psychological impairments should be allowed to be combined in determining if someone suffers from catastrophic impairment.
As a result of a serious single vehicle incident in 2001, Robert Kusnierz suffered numerous physical and psychological injuries including the loss of his left leg below the knee and clinical depression. Due to his disabilities he lost his job and sought accident benefits from his insurance company, Economical Mutual Insurance Company, under the Statutory Accident Benefits Schedule (SABS). While both parties agreed that Kusnierz was entitled to some benefits there was disagreement as to the classification of the injuries sustained and the resulting amount of benefits.
Critique of Proposed Mandatory Helmet Law
Critics of the proposed mandatory helmet law in Ontario suggest that there may be negative repercussions if the government chooses to adopt it. A report from the Office of Ontario’s Chief Coroner which made recommendations on how to reduce the injuries and fatalities of cyclists has prompted debate as to the benefits and concerns of a mandatory helmet law for cyclists of all ages.
While the benefits of wearing a helmet are undeniable there are opponents to such a proposal as it may have an impact of deterring people from cycling, decrease the use of bike-share programs, and also act as a band-aid solution in delaying safety measures such as designated cycling lanes. Such a law may also decrease ‘utility cycling’, such as short trips to the corner store or park.
With a lack of evidence as to the effectiveness and results of mandatory helmet laws the results are uncertain. While the number of serious head injuries in Canada has dropped from 907 in 2001-2002 to 665 in 2009-2010 it is not definitive as to the role that helmet-wearing has played as other safety measures may have also had an impact, such as an increase in bike lanes and safety campaigns.
Currently, for those in Ontario ages 18 and over wearing a helmet is still optional, but of course, highly recommended.
The Ontario Trial Lawyer Association (OTLA), of which Roger R. Foisy is a member, initiated the Bike Helmets on Kids Community Partnership campaign in 2002, which focuses on distributing helmets to children as well as providing education and awareness about helmet use.
To read the full Globe and Mail article please click here.
For more information on the Ontario Trial Lawyers Association please click here.
To read the blog post about the recommendations of the Cycling Death Review by the Office of the Chief Coroner please click here.
Cycling Review Calls for Mandatory Use of Helmets for Cyclists
A report from the Office of Ontario’s Chief Coroner has made recommendations on how to make the roads safer for cyclists.
The recommendations include a ‘complete streets’ approach which focuses on the (re)development of communities by taking into account the safety of all road users, mandatory side guards for trucks which would prevent cyclists from getting caught under the wheels, a one-metre passing rule for vehicles and mandatory helmet legislation for cyclists of all ages.
In the study only 27 per cent of those killed were wearing a helmet.
Currently, in Ontario only cyclists under the age of 18 are required by law to wear a helmet.
In Ontario, where accidents involve a bicycle and a car, cyclists are protected by the Statutory Accident Benefits Schedule, a regulation found in the Ontario Insurance Act. Cyclists need not have their own accident insurance to be provided coverage in these cases.
To view the full article by the Toronto Star please click here.
To view the full Cycling Death Review by the Office of the Chief Coroner please click here.
Understanding What Insurance is Readily Available to You in Ontario After a Car Accident [Video]
What is important to know about automobile insurance coverage after you have been involved in a car accident in Ontario?
The primary concern arising from a motor vehicle collision is to protect your legal rights for any future claims you may have resulting from this collision.
In Ontario, every automobile insurance policy contains mandatory accident benefits coverage.
It is not necessary to be a driver or passenger in an automobile to be eligible for no-fault accident benefits. Pedestrians and cyclists may also be entitled to benefits if they were also involved in the accident. A member of your immediate family who was not in the accident might also be permitted to recover benefits if they have been psychologically or mentally harmed by the cause of events, in some cases.
One of your obligations under the law is to advise your own insurance company about this collision within seven days of the accident. An application for Ontario accident benefits will need to be completed and submitted to your insurance company. This must be done within 30 days of receiving the application package from your insurance company if you or your family members have been injured as a result of this accident.
It is important to carefully read each question and understand specifically what is being asked of you.
Accident benefits can assist you financially with the expenses which will be undoubtedly created if you are injured in an automobile collision.
The key accident benefits available to a person injured in a motor vehicle accident in Ontario include:
Income Replacement Benefits – which partially compensates you for some of the income you may have lost as a result of your inability to return to work due to your injuries;
- Medical and Rehabilitation Benefits – Which will help to pay for medical therapy or treatment, medication, medical equipment, transportation and other rehabilitation needs
- Attendant Care Benefits – Which will compensate for the cost of caring for your personal needs while you are injured
- Visitation Expenses – Which is to reimburse immediate family members for visitation expenses; such as, travel; parking; accommodations; and meals
- Case Management Services – Which is to pay for the medical and rehabilitation coordination of your needs if your injuries have been determined to be catastrophic
There are also other benefits which may be available to you based on the severity of your injuries and whether optional insurance benefits have been purchased by you.
To better understand the benefits available to you following a car accident, you can go to the Financial Services Commission of Ontario’s website. They regulate automobile insurance and provide automobile insurance regulations on their website.
It is also important to remember that you and your family may also have the right to receive compensation from anyone potentially responsible for the motor vehicle collision. This compensation is over and above the Ontario accident benefits you may be entitled to receive.
Accessing the benefits that you are entitled to and protecting your rights against an at-fault party can be very complicated and there are strict limitation periods for commencing law suits. You and your family are well advised to ask an Ontario personal injury lawyer for assistance. Many Lawyers who concentrate in personal injury claims will meet with you free of charge and without obligation.
To learn more about Ontario personal injury law, we invite you to watch our video series that helps answer many of the most common questions asked to Ontario personal injury lawyers.
Supreme Court of Canada Rules that Tree-Falling Fatality is a Motor Vehicle Accident
The Supreme Court of Canada has ruled in the city’s favour after a rotted tree which the city owned fell onto a car killing the driver Gabriel Rossy. Despite the coroner’s report that stated the victim’s death was preventable as the city failed to maintain the rotten tree – in this case by cutting it down – no negligence was found on the part of the city of Westmount, Quebec. Canada’s highest court determined that the victim’s family’s effort to seek compensation should be dealt with through Quebec’s no-fault accident insurance system and not a civil lawsuit against the city.
The Supreme Court of Canada found that this would be classified as an ‘accident’ under Quebec’s no-fault accident insurance scheme. An ‘accident’ under the Automobile Insurance Act, R.S.Q., c. A-25, is an event in which injury or damage was “caused by an automobile, by the use thereof or by the load carried in or on an automobile…” (s. 1, “damage caused by an automobile”). The ‘use’ of the vehicle was it acting as a means of transportation for Rossy when the accident occurred [para 53]. The Court also stated that “the vehicle’s role in the accident need not be an active one. The mere use or operation of the vehicle, as a vehicle, will be sufficient for the Act to apply” [para 52].
In Ontario, the term ‘accident’ under the Statutory Accident Benefits Schedule within the Insurance Act means “an incident in which the use or operation of an automobile directly causes an impairment or directly causes damage…”, but the Supreme Court of Canada has ruled that this should be more broadly interpreted to include the ordinary and well-known uses of an automobile.
To read the full CBC News article please click here.
For the Supreme Court of Canada judgment of Westmount (City) v Rossy, 2012 SCC 30 please click here.
Stay Safe This Summer
With summer now underway many are looking forward to road trips, visits to the cottage, BBQ’s and swimming. Unfortunately, the reality is that during the summer months the top causes for accidental death in Ontario include falls, motor vehicle accidents, alcohol and drug use, and drowning. Using your common sense as you and your family enjoy what summer has to offer means that everyone can stay safe and still have fun.
Refrain from speeding, drinking and driving, and texting while driving. Always wear your seatbelt. When out on the water practice safe swimming and boating practices, such as supervision and the use of life jackets.
While maintaining a safe lifestyle and being a defensive driver will increase your chances of not being involved in an accidental death over the summer, we can never be certain of the actions and irresponsibility of others. If you do get in an accident with an uninsured or underinsured driver then having an umbrella policy through your insurance provider will allow you to access the financial compensation needed to cover medical and rehabilitation expenses. Talk with your insurance representative to see what policy is best for you.
To view the full article by the Toronto Sun please click here.
The Benefits of Having an ‘Umbrella’ Policy in Your Insurance Coverage
When choosing to purchase insurance the option of an ‘umbrella’ policy should be considered. ‘Umbrella’ policies essentially provide extra protection in the event that damages are owed to you due to injuries suffered, such as in a motor vehicle accident. If the at-fault driver does not have sufficient insurance to cover your damages then your own insurer may be able to provide you with the difference created by the shortfall.
‘A Night to Make Music Matter’ Charitable Show
 Music has the power to change lives. That is the belief that gave rise to the organization Make Music Matter (formerly Song for Africa). This registered charity uses music to educate and address human rights issues in struggling African nations and empower those whose lives are affected. Metalworks Institute and Make Music Matter are teaming up to produce a charitable show featuring some of the greatest local musicians, and as an event sponsor Roger R. Foisy encourages anyone interested in the cause or in a night of music to attend.
Music has the power to change lives. That is the belief that gave rise to the organization Make Music Matter (formerly Song for Africa). This registered charity uses music to educate and address human rights issues in struggling African nations and empower those whose lives are affected. Metalworks Institute and Make Music Matter are teaming up to produce a charitable show featuring some of the greatest local musicians, and as an event sponsor Roger R. Foisy encourages anyone interested in the cause or in a night of music to attend.
The students and faculty of Metalworks Institute, a private career college and Canada’s Elite Entertainment Arts School, are producing the July 30, A Night to Make Music Matter, event at Hugh’s Room (2261 Dundas St. W.).
All proceeds from the event will be going to Make Music Matter which is working to build operations in three locations across Rwanda and the Democratic Republic of Congo (DRC) that will tackle a wide variety of developmental and human rights issues including HIV/AIDS orphans, child soldiers and individuals who are survivors of sexual violence.
For more information or to make reservations please click here.
FSCO Against Combining Physical and Psychological Impairments to Determine Catastrophic Impairment
Seriously injured claimants may find it more difficult to access the motor vehicle accident benefits they need if the recent recommendations from Ontario’s insurance regulator are adopted into legislation. The recent report by the Financial Services Commission of Ontario (FSCO) finds that there is no scientific evidence to support the combining of physical and psychological or mental/behavioural impairments for the purposes of determining catastrophic impairment.
This decision comes in direct response to Kusnierz v. Economical Mutual Insurance Company, 2011 ONCA 826, a significant 2011 Ontario Court of Appeal decision, which found the exact opposite. In this case it was held that that it was appropriate to have a more inclusive approach of combining assessments of physical and psychological impairments into one measure as to determine catastrophic impairment. Specifically, if by combining both assessments the claimant has a ‘whole person impairment’ of at least 55 per cent their injuries are classified as catastrophic. Paraplegia, tetraplegia or quadriplegia, severe impairment of ambulatory mobility, blindness, traumatic brain injury, and physical and psychological impairment are all considered to be catastrophic injuries.
(more…)
New Definition of Catastrophic Impairment
Expected Changes to Availability of Auto Accident Benefits with New Definition of Catastrophic Impairment.
With a new and more limited definition of catastrophic impairment potentially going to be implemented by the Ontario government, there is a deep concern that those who suffer serious injuries in motor vehicle accidents will not receive the compensation they need for adequate medical treatment, rehabilitation and support. In other words, it is a great win for insurance companies.
A recommendation report was undertaken by the Financial Service Commission of Ontario (FSCO), a regulatory agency created by the Ontario government. The objective of the report was for FSCO to consult with the medical community and make recommendations primarily on how the definition of ‘catastrophic impairment’ should be amended. (more…)
Should I Hire A Personal Injury Lawyer? [Video]
Should I hire a Personal Injury Lawyer in Ontario or deal directly with the insurance company?
Many people are concerned about lawsuits and are especially fearful about having to testify in a court of law. As a result, injured parties often settle their claim directly with the insurance company before consulting with an experienced injury lawyer.
Is it necessary to consult a personal injury lawyer if you have been in an accident?
As a victim of an accident, there are two things you should immediately be aware of:
1. 95% of all lawsuits settle before they go to trial; therefore, the chances of you having to testify in court are extremely low.
2. When a person negotiates directly with an insurance company, he or she needs to understand that insurance companies have hundreds of years of experience managing and settling losses and as private companies, they are always working for the benefit of its shareholders.
Ontario personal injury lawyers are trained to negotiate fair and reasonable settlements with these insurance companies and are prepared to take them to court if necessary.
While the reality is that very few cases actually go to court, the start of a lawsuit is often necessary to maximize the settlement value needed to reimburse your losses suffered as a result of an accident.
The complexities of personal injury law in Ontario make it very dififcult for the average person to understand what needs be considered before any claim should be settled. It is critical to remember that the maximum settlement value you can achieve is not determined by a simple formula based on your injuries alone.
Insurance adjusters themselves often recommend to the injured party that he/she seek the advice of a personal injury lawyer to fully comprehend all of their options and to help find a suitable solution for their particular case.
This step allows for all of the options to be explored instead of defaulting to a quick settlement with an insurance company.
Ultimately, it is your decision and your decision only, but having all the facts and understanding the full potential of your claim can only improve your chances of achieving a fair settlement value.
To learn more about Ontario personal injury law, we invite you to watch our video series that helps answer many of the most common questions asked to Ontario injury lawyers.
How Ontario Injury Lawyer Fees are Determined [video]
Lawyers are governed by the Law Society of Upper Canada, but that being said, lawyers are not regulated on how much they can charge you on a per hour basis. It is a free market based on experience, as well as supply and demand. There are some exceptions to this rule when it comes to minors and disabled individuals who are always protected by courts pertaining to legal fees.
Personal injury law is different in how lawyers charge clients for their services. It is fair to estimate that at least 95% of personal injury lawyers are paid on a contingency fee basis. This means they only get paid a percentage of what they recover on your behalf.
(more…)
How Personal Injury Settlement Values are Determined in Ontario [video]
How do lawyers come up with personal injury settlement values in Ontario? In other words, how much is your case worth?
There are two critical factors that maximize the value of any settlement:
- Your personal situation
- How your lawyer approaches your case
Your personal situation is of course the most important factor taken into consideration. Factors like your profession, salary, age, severity of injury, expected medical expenses, your medical diagnosis and issues of liability (how the accident came to be) are all factors considered to determine how much you should be fairly compensated.
(more…)
Social Media no Friend to Insurance Litigants
In a recent interview with the Law Times, a leading Canadian Law publication, Roger Foisy warned that insurance companies are looking for evidence online – and in particular in social media platforms to dispute litigant claims. Online media in the form of a picture, video or text may conflict a claims or statement made by individuals on their insurance forms. The primary concern is when a one-time or exceptional event or activity is captured and then interpreted as a lifestyle choice or a reflection of normal abilities. This can cause significant complications for the claimant.
Read the full article
Roger R. Foisy Slams Cost of Medical Records
Roger Foisy was recently interviewed by one of Canada’s leading law publications, the Law Times, on the issue of excessive fees charged by pharmacies and medical offices for providing client medical records. The concern with these charges is they are out of line with the time spent retrieving and providing the information. Roger has been leading the client advocacy on this problem and has sounded the alarm. Eventually, these excessive costs impact clients’ net settlement values and increase costs for insurance companies – ultimately impacting premiums.
Read the full article
Winter Tires: Could You Be Found Negligent?
Did you know that in Ontario you could be found negligent if you are in a car accident in the winter time and found to be driving without winter tires? In the province of Quebec it is actually illegal to drive in the winter time without winter tires. Multiple studies have shown the benefits of winter tires when it comes to slippery road conditions. When it comes to liability, after a car accident if you are sued by someone involved in the accident, you could be found partially responsible for the accident as a result of not having winter tires on your vehicle.
Lawyer Contingency Fee Agreements: Doing it Right
A contingency fee agreement or retainer is defined as an agreement made between the lawyer and their client where the fee for services is only payable when there is a favourable result. This means that the lawyer is not paid until the case is settled in the plaintiff’s favour or a court judgment is arrived at in the plaintiff’s favour. (See Full Legal Glossary of Terms)
Conflicting Limitation Periods for Car Accident Insurance Claims
The car accident insurance case, Whorpole Estate v. Echelon General Insurance Co., [2011] O. J. No. 1644 (S. C. J.) has brought up the issue of conflicting limitation periods, where more than one limitation period exists and a decision must be made over which applies. In particular, this case shows the conflict between a limitation period according to the Trustee’s Act and one according to the Insurance Act.
Defining ‘Minor Injury’ in Personal Injury Motor Vehicle Cases
In September 2010, the Ontario Liberal government dramatically reduced the amount of medical and rehabilitation benefits available for injured people. For most Ontario car accident victims, the amount of available rehab money dropped from $100,000 to $3,500 with the introduction of the Minor Injury Guideline (MIG).
Immediately After a Motor Vehicle Accident
Immediately after a car accident or other motor vehicle accident there are few important things you need to consider:
Keep your composure: It is important that you remain calm. Do not argue with other drivers and passengers. Save your story for the police. Do not leave! If you leave the scene of an accident you may be subject to criminal prosecution. Do not voluntarily assume liability or take responsibility, sign statements regarding fault, or promise to pay for damage at the scene of the accident.
Insurance Does Not Mean You Cannot Be Sued
If you have car insurance this does not mean that you can’t still be sued personally if you are involved in a car accident. Your insurance company will only cover you up to the amount of insurance coverage you have. Many people are under the impression that they purchase insurance to protect themselves from being sued and losing their home.
What are No Fault Insurance Benefits?
There is a common misconception that ‘no fault’ insurance means that after a car accident no one is held to be at fault. This is not the case and the expression ‘no fault’ can be somewhat misleading when it comes to injuries resulting after a motor vehicle accident.
When someone is involved in a car accident with another driver, both individuals are required by law to be carrying automotive insurance. The law also requires that every insurance policy contain, by default, standard accident benefits. Additional insurance benefits can be purchased but every insurance policy will contain these standard ‘no fault’ insurance benefits.
Immediately After a Car Accident
Immediately after a motor vehicle accident, families may often find themselves having difficulties dealing with the sometimes overwhelming emotions they feel for the loved one involved in the car accident. It is at this moment, during the crisis, that things like taking care of making phone calls, helping to arrange childcare, providing compassion by holding their hand and listening to the ones affected by the accident are so important.
Organizations like the “Victim Assistance Volunteer Program” offered by the Burlington Ontario Provincial Police are crucial. They provide community-based short term emotional support and practical assistance to victims of car accidents and their loved ones through the use of specially trained volunteers. Their goal is to help victims and their families cope during these types of crisis situations within the first few hours in which they occur. In addition to providing the types of compassionate services mentioned above, these organizations can also provide important referrals necessary to help the family deal with the immediate situation and the events that follow.
I thought “AB” was just two letters in the alphabet and “Tort” was some kind of Pie?
After a car accident has claimed the life of a family member, individuals will seek legal advice to determine whether or not they can sue the driver of the other vehicle. A lawyer may during a free initial consultation inform the family members of two major aspects of any case. After a fatal car accident the majority of cases will have an accident benefits claim (usually termed as an “AB claim”) and a claim as against any at fault parties (usually termed as a “Tort claim”).
The AB (Accident Benefits) claim relates to matters relating to the no-fault aspect of the motor vehicle accident. These claims are generally covered by your no-fault insurance benefits and can cover items such as medical, rehabilitation, funeral expenses, etc. As noted in a previous blog, every car insurance policy by law in Ontario will have a ‘no fault’ accident benefits component by default. This part of the claim typically involves your insurance company only.
Facebook, YouTube, Twitter and other Social Networks – Risky Business?
When it comes to companies providing you with insurance, the job of the ‘underwriter’ is to assess the risk you present to the insurance company should they decide to insure you. Things like age, drinking, smoking, medical history, family history of medical issues etc… may be taken into consideration when determining how “risky” a client you may be. This also determines how much your insurance premiums will be. Insurance companies at the end of the day are looking to make money and to do so means paying out the least amount of money possible.
These days, beyond the medical and application form/questionnaire, insurance companies are turning to social networks to obtain further information. Is your profile open for others to see? Do you post things like your interests in bungee jumping or sky diving? Do your pictures show you smoking when you told the insurance company you didn’t? How about your latest “party” or “binge drinking episode”? Posting personal information on Facebook, YouTube, Flickr Linked-in, MySpace, Twitter or other social venues may provide the insurance company with additional information to determine you are a higher risk client than suggested by your medical exam or application.
Putting a Stop to Phantom Clients Forever
The courts have made a distinction between a solicitor-client relationship and a solicitor-client retainer. The relationship is established when the prospective client has his or her first consultation with the lawyer or law firm about retaining services. The relationship is often established without formality.
The retainer is established once the lawyer agrees (expressly or implied by the lawyer’s conduct) to provide legal services. Until it is made clear by way of a non-engagement letter to the prospective client, it may be that a solicitor-client relationship, with all of its important duties, truly does exist.
Case Study in Point
Eight months ago Mr. Smith consulted with Lawyer Jones with respect to a personal injury matter. Lawyer Jones met with Mr. Smith for a half hour free consultation after which time he advised Mr. Smith about what he believed to be the answer to his motor vehicle accident issue. He made sure to tell Mr. Smith that he probably could find a more experienced lawyer as he had not practiced in this area of law for years. Nothing else was done by Lawyer Jones. Today he received a message left on his voice mail from Mr. Smith looking for his trial date. Lawyer Jones looks at his notes from eight months past and realizes that Mr. Smith’s motor vehicle accident itself was just over two years ago.
Is File Handling one of Your New Year`s Resolutions?
You enter your office and you sit at your desk. A letter addressed to you “personal and confidential” stares you in the face. You open it and read the allegations against you. You feel personally and unjustifiably attacked. Your hands perspire and you call for the file to reassure yourself that this letter has no merit. Your assistant hands you the file. You cancel your appointments so you can deal with this. At the end of the day, feeling exhausted, you pick up the letter one more time and question why you chose to represent a client on a matter outside of your area of expertise.
Unfortunately this story is not fiction. Some lawyers were unfortunate enough to receive this letter in 2010. One of their New Year’s Resolutions is now: “Think twice before accepting retainers for any client who comes asking for your help.”
If any of these files include personal injury or disability insurance matters, my office is more than willing to assist. Any lawyer who may have realized over time that they require additional expertise in one of these areas of law, or who may need a quick second opinion, should feel free to contact me.
Young People and Fatal Car Crashes – Too Easily Becoming A Statistic
Car Crashes are the leading cause of death for teens or young adults in Canada and in the United States. In Canada, Statistics Canada reported that from the years 2000 through to 2004, motor vehicle crashes causing death accounted for 1.3% of all deaths in Canada; however, 17.3% of all deaths among Canadians younger than 30 years old. The research also showed that males consistently had higher motor vehicle accident deaths than did females.
In the US, the Centers for Disease Control, reported that each year over 5,000 teens ages 16 to 20 die due to fatal injuries caused car accidents. It further reported that about 400,000 drivers age 16 to 20 will be seriously injured.
In summary, teenagers are about 10 percent of the US population but account for 12 percent all fatal car crashes.
Should you be Increasing Your Automobile Liability Coverage
Most Ontario automobile owners purchase higher third party insurance liability limits than the mandatory minimum coverage of $200,000. However, I suggest that the reason a consumer chooses higher coverage (usually $500 thousand or $1 million) is only due to the fact their insurance agent suggests this amount will help keep the overall automobile insurance premium down.
While your insurance representative will be able to help you decide what level of coverage is best for you, it helps to be well-informed about what is available to you before making that call.
The current Ontario law requires that each motor vehicle owner carry a minimum of $200,000. This minimum amount has been in place for decades in Ontario despite the fact that injury awards have increased to keep up with inflation over the years. Take for example, if you were found at-fault for a motor vehicle accident back in 1978 and rendered an accident victim such as a quadriplegic, the courts would have awarded the injured victim approximately $100,000 for pain and suffering. Of course this award would not include other losses for possible past and future medical and/or income losses.
Car accident benefits – It is time to pay attention to your auto policy!
Car accident benefits have been slashed up to 50% and some benefits have been eliminated — how will accident victims be able to cope?
My clients almost always tell me that before their car accidents, they thought insurance was both boring and confusing. For these reasons they decide to put their insurance coverage at the bottom of their priority list.
This fall, car insurance is moving from the back burner to the front burner. Despite the confusing nature of the insurance contract itself and whether or not anyone could ever spare the time to read all of the fine print contained within an insurance policy, here is what everyone needs to pay attention to:
New Drinking And Driving Measures May Help To Prevent Fatalities
Ontario is making the province’s roads safer for all Ontarians with new changes that will help protect young and novice drivers.
Starting August 1, all drivers 21 years of age and younger must have a zero blood alcohol level when they get behind the wheel or face:
- An immediate 24-hour licence suspension
- 30-day licence suspension
- Up to $500 in fines
How does Ontario measure up in Canada when it comes to motor vehicle accident deaths?
The Ontario Government and Ontarians alike have been suggesting that fatal car accidents have been on the rise. Despite the ever-increasing number of vehicles on the roads, half as many Canadians were killed in a motor vehicle accident in 2004 as there had been 25 years earlier according to Statistics Canada study published.
The study “Motor vehicle accident deaths, 1979 to 2004,” published today in Health Reports showed that during the past quarter-century, 97,964 people were killed in motor vehicle accidents. The annual number of deaths fell 52% from 5,933 in 1979 to 2,875 in 2004.
Sharp declines were detected even after adjusting for the aging of the population, suggesting that factors other than demographics are behind the drop. Almost three-quarters (71%) of the people who died in these accidents were male.
Strongly consider increasing your No-fault Insurance Benefits – What you need to know about changes to auto insurance in Ontario
The Ontario government is introducing significant reforms to the auto insurance system, if you have never taken the time to consider the differences you can expect from your now Standard Auto Insurance Policy and what it will look like on September 1, 2010, it is imperative you take the time NOW:
Standard Auto Insurance Policy
All auto insurance policies will continue to include the following:
Third‐Party Liability
Uninsured Auto coverage
Direct Compensation‐Property Damage
Statutory Accident Benefits
In addition, if you previously purchased Collision and/or Comprehensive coverage, it will still be included in your policy.
The McGuinty Government’s New Changes to the Ontario Auto Insurance Regulations in the fall of 2010
A Quick Summary of the Changes
Accident benefits for non-catastrophic injury claims will undergo some major changes, including:
• Caregiver Benefits – The $250 per week, plus $50 per additional person in need of care will be eliminated
• Medical and Rehabilitation Benefits – These benefits are being reduced to $50,000 from $100,000
• Attendant Care Benefits – These benefits will be reduced to $36,000 from $72,000 per annum
• Housekeeping Benefits – The $100 per week housekeeping benefit will be eliminated
Accident benefits for catastrophic injury claims will undergo some major changes, including:
• Treatment assessment costs will be deducted out of the specific benefit limit
• There will be no ability to apply for Catastrophic designation (whole person impairment test or the marked/extreme mental or behavioural test) in the first two years post-accident, except in cases where a brain injury is present
• There will incur a definition for “incurred” which will require the insured person to pay for the expense, and the service provider to be a professional provider, except in cases of family members whom are able to prove loss of income
• Assessment costs are limited to $2,000
Personal Injury Law and Social Media
Beware personal injury and insurance clients when it comes to social media sites like FaceBook, MySpace,YouTube and many other sites which are popping up every day.
Posting personal information about yourself and your immediate family members including photographs or video can easily undermine plaintiffs’ lawsuits. Insurance companies and their investigators have become well versed in many techniques to weaken plaintiffs’ cases and social media has become a favourite investigative tool.
Ontario courts are more routinely ordering injured plaintiffs to produce their Facebook or other social media pages to insurance company lawyers. These courts have also recently admitted FaceBook pages into evidence.
Fibromyalgia & Chronic Fatigue Syndrome Disability Claims
Fibromyalgia and Chronic Fatigue Syndrome can be devastating disabilities to experience.
Fibromyalgia is a rheumatic disease resulting in a number of symptoms, including pain tender/trigger points, difficulty with sleeping, concentration and a host of other symptoms. Fibromyalgia can affect both adult women and men.
Chronic fatigue syndrome is characterized by a prolonged, debilitating lack of energy that leaves some individuals the inability to leave their own bed. Both conditions can be long-lasting, chronic, and severely disabling medical conditions.
Keep Insurance Up-dated for Peace of Mind
Planning on lots of driving this summer?
Heading up to the cottage this summer? Planning on a “see Canada” road trip vacation? A tune-up for your car before any big driving vacation is always a good idea but what about a “tune-up” for your insurance?
Before you pack, it’s always a good idea to check your insurance policies. The driving risks for cottager commuters, who spend many hours behind the wheel, increase during the summer months.
Unfortunately, the fun and relaxation for cottagers is sometimes overshadowed by the additional risks. Not only are there the driving risks on the road, but there is always the possibility of mishaps which can easily occur on the water or with a fire pit that accidently gets out of control. Many people are dismissive about mishaps, thinking that they always happen to other people.
Are You Increasing Your Liability Insurance Coverage?
Should you be Increasing Your Liability Coverage?
Most Ontario automobile owners purchase higher third party insurance liability limits than the mandatory minimum coverage of $200,000. However, I suggest that the reason a consumer chooses higher coverage (usually $500 thousand or $1 million) is only due to the fact their insurance agent suggests this amount will help keep the overall automobile insurance premium down.
While your insurance representative will be able to help you decide what level of coverage is best for you, it helps to be well-informed about what is available to you before making that call.
Motor Vehicle Insurance Housekeeping Benefits
Housekeeping and Home Maintenance Benefits – What you need to know about your Insurance Policy Accident Benefits if you have been involved in a motor vehicle collision
Many individuals who have suffered injuries as a result of a motor vehicle accident in Ontario have come to realize that their injuries have affected their ability to carry-on with housekeeping and home maintenance in the same manner which they were accustomed to before their car accident.
Under the current Ontario Insurance Act, Statutory Accident Benefits Schedule, an accident victim is entitled to claim assistance from their own accident insurer if a health care provider confirms that they are unable to substantially perform the housekeeping and home maintenance services they normally performed before the accident. In this situation, an insurer shall pay up to $100 per week for reasonable and necessary additional expenses incurred by or on behalf of an insured person. These benefits were available to insured persons for 2 years from the date of their automobile accident.

 Profile: Roger R. Foisy is an experienced Ontario Personal Injury Lawyer helping accident victims and their families in Mississauga, Milton, Georgetown, Brampton, Oakville, Cambridge, Guelph, Kitchener-Waterloo and surrounding areas. Roger and his team dedicate a very personal level of attention to each and every client in their care and maximize clients’ personal injury settlements.
Profile: Roger R. Foisy is an experienced Ontario Personal Injury Lawyer helping accident victims and their families in Mississauga, Milton, Georgetown, Brampton, Oakville, Cambridge, Guelph, Kitchener-Waterloo and surrounding areas. Roger and his team dedicate a very personal level of attention to each and every client in their care and maximize clients’ personal injury settlements. 






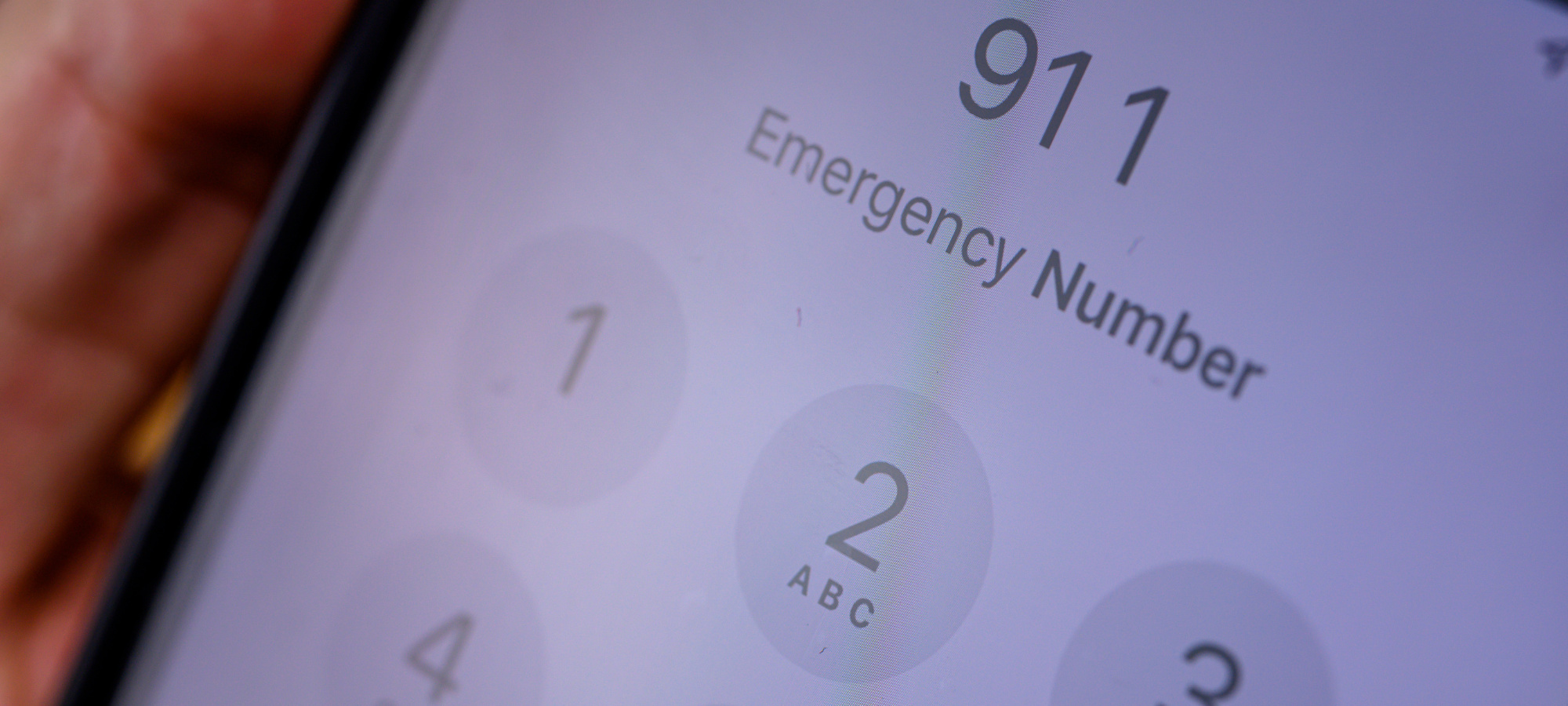





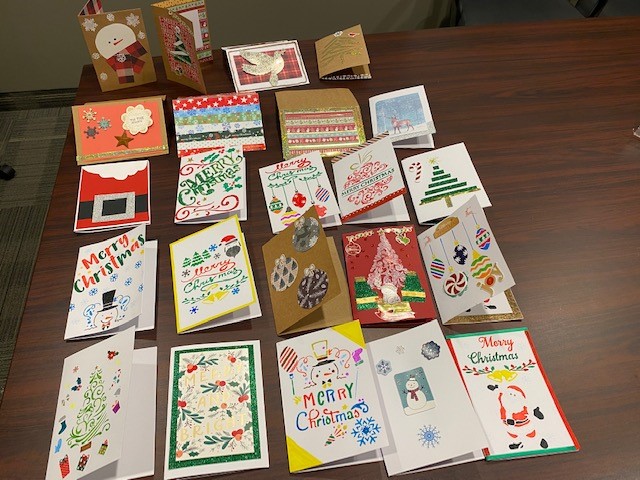













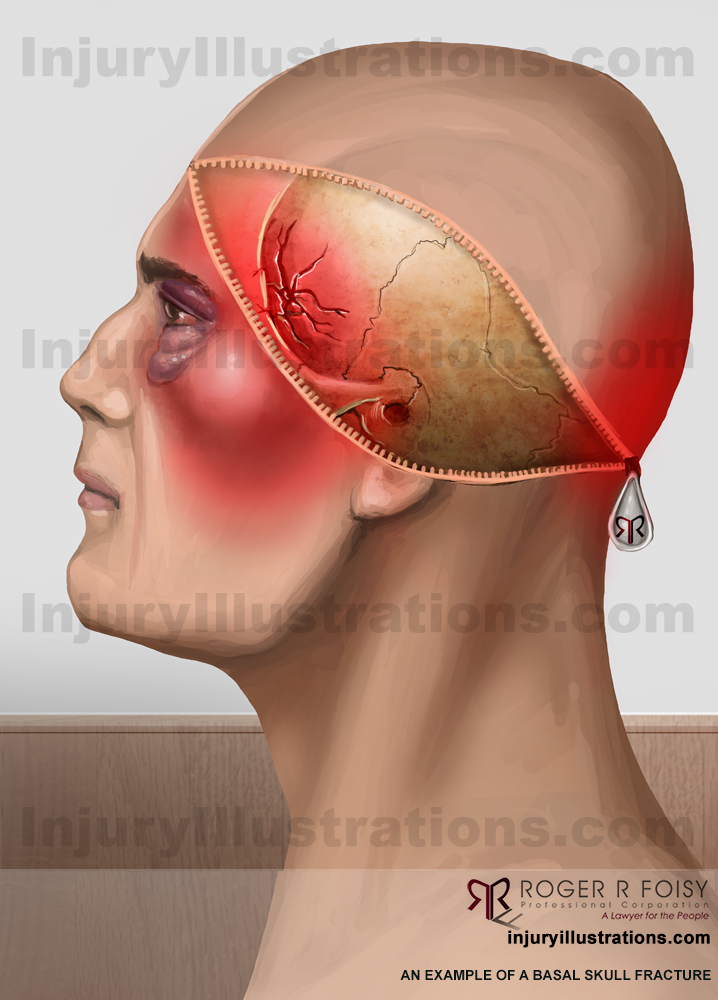
 The first thing you need to know is that concussions are mild traumatic brain injuries (mTBI). Do not let the word “mild” fool you; nothing about any brain injury is “mild”.
The first thing you need to know is that concussions are mild traumatic brain injuries (mTBI). Do not let the word “mild” fool you; nothing about any brain injury is “mild”.